Whiplash injury is an inertial mechanical injury. Consequently, chiropractors, as a consequence of the mechanical nature of their clinical practice, treat many whiplash-injured patients. Although chiropractors manage a wide range of clinical syndromes and findings, the emphasis of chiropractic clinical practice is to treat, primarily through spinal adjusting, regions of spinal hypomobility (less than normal motion). However, chiropractors are well aware that spinal trauma may also cause regions of hypermobility (excessive motion).
In the evaluation of an injured patient, chiropractors assess the spine for both hypomobility and hypermobility.
Hypomobility is classically managed with spinal adjusting, myotherapy, stretching exercises, and modalities that reduce spasm.
Hypermobility is classically managed by applying spinal adjusting to adjacent hypomobile joints, varying forms of immobilization, and resistive effort exercises.
Chiropractors are aware that trauma, especially whiplash trauma, can result in a risk to the integrity of the nervous system. This type of hypermobility is referred to as Clinical Instability. Clinical Instability management may require prolonged immobilization, or on occasion a surgical stabilization. This paper reviews the historical and contemporary perspectives on Clinical Instability.
•••••
Clinical Instability was first defined by Augustas A. White, MD, and Manohar M. Panjabi, PhD. Dr. White is Professor of Orthopedic Surgery at Harvard Medical School, as well as Orthopedic Surgeon-in-Chief at Beth Israel Hospital in Boston. Dr. Panjabi is Professor of Orthopedics and Rehabilitation at Yale University School of Medicine.
In the Second Edition (1990) of their authoritative text, Clinical Biomechanics of the Spine, they define clinical instability as (8):
“Clinical Instability is the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no matter major deformity, and no incapacitating pain.”
White and Panjabi also state:
“The major practical consideration in the determination of clinical instability is the evaluation of the patient’s radiographs.”
“Radiographic examination is the most often used objective means of determining the relative positions of the vertebrae in a potentially unstable spine. Therefore, it is important to give some consideration to the accurate interpretation of linear radiographic measurements.”
•••••
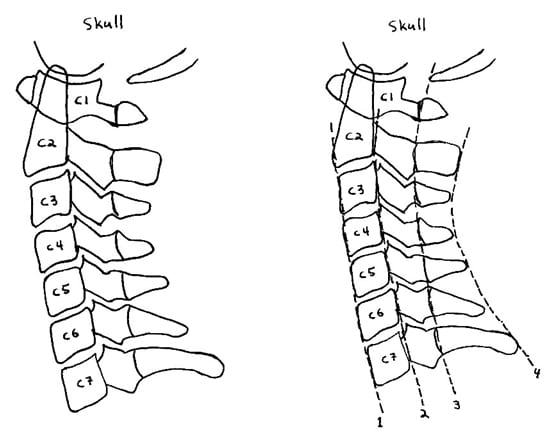
The radiographic evaluation primarily involves the lateral cervical views, beginning with the neutral lateral cervical x-ray. The first picture below is a representative lateral cervical view with the patient facing to the left. According to radiologist Amil Gerlock, MD, and colleagues, the structural integrity of the lateral cervical radiograph is best visualized by adding four contour lines (second picture below), as follows (9):
1) The line drawn on the anterior margins of the vertebral bodies. This line should be a smooth and gentle curve, convex anteriorly.
2) The line drawn on the posterior margins of the vertebral bodies. This line should also be a smooth and gentle curve, convex anteriorly. This line represents the anterior margin of the spinal canal, where the spinal cord resides.
3) The line drawn on the bases of the spinous processes. This is also known as the spinolaminal line. This line should also be a smooth and gentle curve, convex anteriorly. This line represents the posterior margin of the spinal canal, where the spinal cord resides.
4) The line drawn on the tips of the spinous processes from C2 to C7. This line should also be a smooth and gentle curve, convex anteriorly. This line represents the anterior margin of the spinal canal, where the spinal cord resides.
Any break in the smooth continuity of any of these lines is an indication of soft-tissue injury and the potential for clinical instability.
In March 2009, the journal Sports Biomechanics published a study using a detailed three-dimensional finite element model of the human cervical spine to study flexion and extension injuries to the cervical spine. The authors, Abraham Tchako and Ali Sadegh, are mechanical engineers from Union College in New York and City University of New York. The article is titled (1):
A cervical spine model to predict injury scenarios and clinical instability
The authors were able to establish that motor vehicle injuries to the cervical spine can cause clinical instability. However, they also note that cervical spine clinical instability cannot be documented with a clinical examination, and that specific imaging studies are required.
The authors note that the standard for the assessment of clinical instability was established by Augustas A. White, MD, and Manohar M. Panjabi, PhD. Dr. White is Professor of Orthopedic Surgery at Harvard Medical School, as well as Orthopedic Surgeon-in-Chief at Beth Israel Hospital in Boston. Dr. Panjabi is Professor of Orthopedics and Rehabilitation at Yale University School of Medicine.
These authors also state:
“The cervical discs are relatively small compared with the discs in the other parts of the spinal column. Consequently, the exiting space for the nerves is also small, which means that even a small abnormal disc material displacement may encroach on the nerve and cause significant pain.”
“Some radiologists in the US consider a 2-mm anterior displacement to be the average displacement for instability.”
“Clinical studies have shown that about 35% of cases of herniated discs in the cervical spine go undetected.”
•••••
From a clinical and medical-legal perspective, clinical instability is quite important. Clinical instability implies substantial injury, poor recovery, impairment and disability. One study notes that up to 30% of those with clinical instability “may suffer permanent neurologic sequelae (2).”
The primary motor vehicle collision injury is to the facet joint capsules (3), and facet injury alone can cause clinical instability (7). However, it is established that the injury can extend to involve the intervertebral disc (4), and also the anterior longitudinal ligament (5). Injuries to the intervertebral disc and anterior longitudinal ligament are more serious than facet capsular injuries, and are much more likely to result in clinical instability.
Historically, clinical instability is assessed with stress radiography. In the cervical spine, this typically includes neutral lateral cervical, maximum flexion lateral cervical, and maximum extension lateral cervical x-rays. In 2003, Spine published an article titled (6):
Increased sagittal plane segmental motion in the lower cervical spine in women with chronic whiplash-associated disorders, grades I-II: a case-control study using a new measurement protocol
This article states:
“Flexion-extension radiography has been in clinical use for over 50 years to detect abnormal segmental motions in the spine.”
•••••
As noted above, Harvard’s Augustas White, MD, and Yale’s Manohar Panjabi, PhD, established the standard for the assessment of clinical instability. Their initial article was published in the journal Clinical Orthopaedics and Related Research in June, 1975, and titled (7):
Biomechanical analysis of clinical stability in the cervical spine
In this paper, the authors performed detailed experiments and analysis of the effects of destroying ligaments and facets on the stability of the cervical spine below C2. Their primary protocol involved analysis of maximum flexion and extension x-rays. They note that cervical spine muscles do not play a significant role in clinical stability; rather clinical stability is primarily as a consequence of ligamentous integrity.
In their biomechanical analysis, White and Panjabi state:
“If acute horizontal displacements exceeding 3.5 mm are found on standard [neutral] lateral roentgenograms of the neck in the acutely injured adult population, this motion can be considered as abnormal and indicates that the spine is unstable.”
In addition, White and Panjabi state:
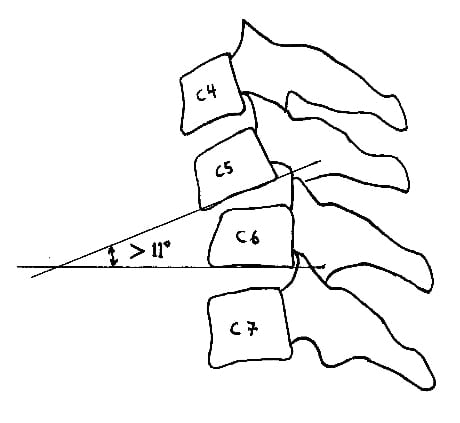
“If there is angulation of the vertebrae in question that is more than 11 degrees greater than the angulation of either normal adjacent vertebrae then the excessively rotated vertebrae is unstable.”
White and Panjabi emphasize the importance of the integrity of the facet joints, stating:
“The prospect of clinical instability in horizontal translation is significantly greater following the loss of the functional integrity of the facets.”
White and Panjabi summarize their work by stating that if either of these two conditions exist, the spine is “unstable or on the brink of instability:
1) “More than 3.5 mm horizontal displacement of one vertebrae in relation to an adjacent vertebrae, anteriorly or posteriorly, measured on resting [neutral] lateral or flexion-extension roentgenograms of the spine.”
2) “More than 11 degree of rotational differences to that of either adjacent vertebrae, measured on a resting [neutral] lateral or flexion-extension roentgenogram.”
•••••
Although Augustas White, MD, and Manohar Panjabi, PhD, first described the evaluation of clinical instability in 1975 (7), their core analysis remained unchanged 15 years later when they published the Second Edition (1990) of their authoritative text, Clinical Biomechanics of the Spine. In the past 20 years, since 1990, there have been a few updates as to the assessment of clinical instability that vary slightly from the original work of White and Panjabi, as follows:
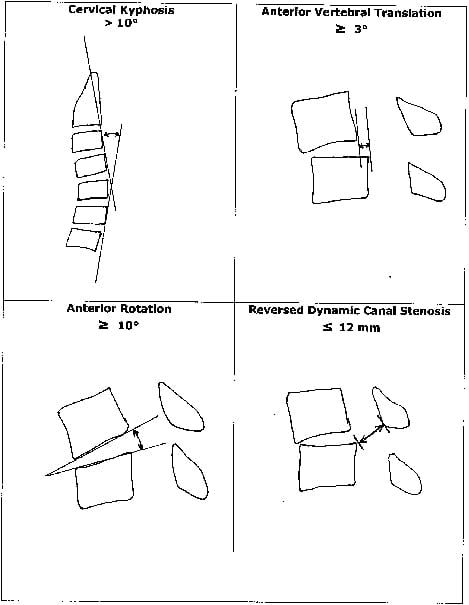
• In 2009, researchers from the Department of Orthopaedics and Rehabilitation Medicine, Fukui University, Japan, list four criteria as being indicative of spinal clinical instability (10):
1) Cervical spine kyphotic deformity of > 10 degrees. This criterion was not included in the original work of White and Panjabi.
2) A cervical disc angle of anterior rotation > 10 degrees. This is slightly different than the original analysis of White and Panjabi. White and Panjabi measured the angle formed between two adjacent inferior vertebral body end plates; these authors measured the actual disc angle.
3) Anterior vertebral translation of 3 mm. The analysis is identical to the original work of White and Panjabi, but they reduced the threshold from 3.5 mm to 3 mm.
4) They add reversed dynamic canal stenosis to less than 12 mm as being indicative of spinal clinical instability. This criterion was not included in the original work of White and Panjabi.
• In 2001, researchers from Wayne State University School of Medicine in Dayton, Ohio, published a study indicating that the protocols set forth by White and Panjabi could miss some clinically important cases of cervical spine clinical instability (2). Their study indicates that an improved method of investigation involves dynamic fluoroscopy (motion x-rays) with lateral cervical flexion/extension views. Their study was published in the journal Current Surgery.
• Researchers from Nova Southeastern University College of Medicine in Winter Springs, Florida have published a number of studies indicating that the most effective way to assess clinical instability and other injuries following whiplash trauma involves the utilization of kinematic cervical spine magnetic resonance imaging (11, 12, 13). The protocols they describe involve the use of flexion/extension motion MRI of the cervical spine.
•••••
On July 29, 2010, Malik Slosberg, Dc, MS, published a review article
titled (14):
How Spinal Manipulation Activates Segmental Stabilization of the Spine
Dr. Slosberg is a full professor at Life Chiropractic College West in
Hayward, California. In this article, Dr. Slosberg documents the following model of how chiropractic adjusting can improve segmental spinal instability:
Tissue injury and pain results in reflex inhibition and progressive atrophy of the segmental multifidus muscle.
The chiropractic adjustment rapidly stretches ligaments, joint capsules and intervertebral discs, stimulating stretch receptors, and initiating a ligamentomuscular reflex, which activates the segmental multifidus to stabilize and protect passive ligamentous restraints from injury.
The segmental multifidus that has been reflexly inhibited and atrophying is stimulated to contract.
This may reverse the reflex inhibition, progressive atrophy, and delayed muscle response in the segmental multifidus, and restore contractility and improve dynamic joint function.
The key concept from Dr. Slosberg is that chiropractic spinal adjusting can improve spinal segmental instability as a consequence of activating the multifidus muscle.
•••••
Spinal clinical instability is a concept that is well understood by chiropractors. All spinal trauma patients, especially whiplash trauma patients, should be assessed for spinal clinical instability. For decades, this assessment has been done primarily by using maximum flexion and maximum extension lateral cervical x-rays, and this service is routinely performed on spine trauma patients by chiropractors. For clinical reasons, some patients may need additional assessment, more than dynamic radiography. In these cases, it is suggested that the patient be referred for either dynamic fluoroscopy or dynamic MRI.
Spinal clinical instability patients have greater injury and a worse prognosis for complete recovery. Chiropractors have a number of conservative approaches in the management of the spinal clinical instability patient. If appropriate improvement is not obtained within a reasonable timeframe with conservative management, these patients can be referred for a surgical stabilization consultation.
REFERENCES
1) Tchako A, Sadegh A. A cervical spine model to predict injury scenarios and clinical instability; Sports Biomechanics, March 1009; 8(1): 78-95.
2) Cox MW, McCarthy M, Lemmon G, Wenker J. Cervical spine instability: clearance using dynamic fluoroscopy. Current Surgery. January 2001;58(1):96-100.
3) Pearson AM, Ivancic PC, Ito S, Panjabi MM. Facet joint kinematics and injury mechanisms during simulated whiplash. Spine (Phila Pa 1976). 2004 Feb 15;29(4):390-7.
4) Panjabi MM, Ito S, Pearson AM, Ivancic PC. Injury mechanisms of the cervical intervertebral disc during simulated whiplash. Spine (Phila Pa 1976). 2004 Jun 1;29(11):1217-25.
5) Ivancic PC, Pearson AM, Panjabi MM, Ito S. Injury of the anterior longitudinal ligament during whiplash simulation. Eur Spine J. 2004 Feb;13(1):61-8.
6) Kristjansson E, Leivseth G, Brinckmann P, Frobin W. Increased sagittal plane segmental motion in the lower cervical spine in women with chronic whiplash-associated disorders, grades I-II: a case-control study using a new measurement protocol. Spine (Phila Pa 1976). 2003 Oct 1;28(19):2215-21.
7) White AA 3rd, Johnson RM, Panjabi MM, Southwick WO. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res. 1975;(109):85-96.
8) White AA, Panjabi MM. Clinical Biomechanics of the Spine; Second Edition, Lippincott, 1990.
9) Gerlock AJ, Kirchner SG, Heller RM, Kaye JJ. The Cervical Spine in Trauma; Suanders, 1978.
10) Kenzo Uchida, M.D., Ph.D., Hideaki Nakajima, M.D., Ph.D., Ryuichiro Sato, M.D., Ph.D., Takafum i Yayama, M.D., Ph.D., Erisa S. Mwaka, M.D., Shigeru Kobayashi, M.D., Ph.D., and Hisatoshi Baba, M.D., Ph.D. Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment: Outcome after Anterior or Posterior Decompression; Journal of Neurosurgery: Spine; November 2009, Volume 11, pp. 521-528.
11) Giuliano V, Giuliano C, Pinto F, Scaglione M. The use of flexion and extension MR in the evaluation of cervical spine trauma: initial experience in 100 trauma patients compared with 100 normal subjects. Emerg Radiol. 2002 Nov;9(5):249-53.
12) Giuliano V, Giuliano C, Pinto F, Scaglione M. Soft tissue injury protocol (STIP) using motion MRI for cervical spine trauma assessment. Emerg Radiol. 2004 Apr;10(5):241-5.
13) Giuliano V, Pinto A, Scaglione M. Kinematic cervical spine magnetic resonance imaging in low-impact trauma assessment. Semin Ultrasound CT MR. June 2009 ;30(3):168-73.
14) Slosberg M. How Spinal Manipulation Activates Segmental Stabilization of the Spine; Dynamic Chiropractic; July 29, 2010.

![“If acute horizontal displacements exceeding 3.5 mm are found on standard [neutral] lateral roentgenograms of the neck in the acutely injured adult population, this motion can be considered as abnormal and indicates that the spine is unstable.”](https://chiro-trust.org/wp-content/uploads/2014/03/Untitled-3524-copy.jpg)