Pain is a brain cortical event. Pain does not exist in a back or neck or foot. Pain is perceived by brain cortical neurons. Any intervention that reduces pain is altering the electrical signal depolarization of brain cortical pain perceiving neurons. As stated by Drs. Heidi Haavik-Taylor and Bernadette Murphy in 2007 (8):
“Spinal manipulation is a commonly used conservative treatment for neck, back, and pelvic pain.”
“The effectiveness of spinal manipulation in the treatment of acute and chronic low back and neck pain has been well established by outcome-based research.”
In 2011, Ogura and colleagues state (9):
“Chiropractic spinal manipulation is an alternative treatment for back pain.”
“Research on chiropractic spinal manipulation has been extensively performed worldwide, and its efficacy on musculoskeletal symptoms has been well documented.”
••••
Spinal manipulation has been used to treat a variety of syndromes for millenniums. In his 1982 book, orthopedic surgeon James Cyriax, MD, presented evidence of spinal manipulation being performed 2000 years ago in Thailand, 2000 years ago in Libya, and 2300 years ago in Mexico. He also presents early evidence from Turkey and Italy (1).
Sophisticated refinements of spinal manipulative diagnostics and techniques began in 1895 with the beginning of chiropractic as a profession. Soon thereafter, these spinal manipulative diagnostic and adjustive techniques were being taught throughout the United States in chiropractic colleges.
State licensure for the practice of chiropractic began in Kansas in 1914; the final state to license chiropractic was Louisiana in 1974.
In the early 1970s, the United States Department of Education (actually is was HEW back then, for Health, Education, and Welfare) recognized the Council on Chiropractic Education as an accrediting agency for chiropractic education. Along with this recognition came reimbursement under Medicare. Today chiropractic services are recognized and reimbursed by Medicare, Veteran’s Affairs (military), Worker’s Compensation, Personal Injury (automobile insurance), and most private health insurance policies.
Cooperation between the chiropractic profession and the medical profession struggled until the final verdict of the chiropractic antitrust lawsuit against the American Medical Association concluded in 1987. Since then essentially all chiropractors work closely with medical providers, referring patients between them in the best interest of the patient’s well being.
••••
In chiropractic’s infancy, public health officials and legislative bodies noted that people under chiropractic care often had improvement of problems that were not considered to be musculoskeletal in origin. Specifically, in the 1920s and the 1930s, public health officials and legislative bodies started to document improvement of brain function in mentally ill patients who came under chiropractic care.
For example, in 1931, the Kentucky House of Reform presents a series of 244 adolescent boys who were incarcerated by the State of Kentucky because of criminal or behavioral problems in the year 1931 (2). The report documents that “almost 100 per cent have shown improvement in conduct, and “144 of our 244 patients have been paroled since we have been giving them Chiropractic treatment.”
The Report states:
“IN ADDITION TO REGULAR PHYSICIANS EMPLOYED AT THE INSTITUTION WE HAVE HAD THE SERVICES OF CHIROPRACTORS. ALLOW ME TO SAY THAT I FEEL THE FINE SHOWING IN THE NUMBER OF PROMOTIONS AND DISMISSALS FROM THE INSTITUTION IS LARGELY ATTRIBUTABLE TO THE VERY EXCELLENT WORK DONE BY THE CHIROPRACOTORS WHO HAVE ALMOST DAILY LOOKED AFTER THE HEALTH AND GENERAL WELFARE OF THESE BOYS.” [these words were capitalized in the reference]
Another example is the legal briefs presented to the 1935 session of the North Dakota Legislature by the Honorable Judge A.W. Ponath (3). Judge Ponath was County Judge of the Probate Court of Richland County, Wahpeton, North Dakota. Judge Ponath’s legal briefs present 44 cases where mentally ill patients were treated chiropractically in the Jamestown State Insane Asylum (North Dakota). Twenty-seven of the 44 cases “have either been cured or sufficiently recovered so that they can remain at home and resume their former responsibilities [61%].” Judge Ponath notes that these “patients who had for the most part had already spent considerable time in asylums or sanatoriums,” and “in many cases had been declared incurable” by Medical Authorities. Judge Ponath notes that 70-75% of such institutionalized persons are doomed to an asylum prison for life.
How are such claims biologically possible? What are the biologically plausible explanations for such observations?
••••
The science of chiropractic (and traditional osteopathy) advanced significantly as a consequence of the efforts of Irvin M Korr, PhD (1909-2004, age 94). It is rare for any person to have their obituary included in the National Library of Medicine database, yet Dr. Korr’s can be found twice (4, 5).
Dr. Korr was a graduate of the University of Pennsylvania and he earned his doctorate in physiology at Princeton University. His obituary states (5):
Dr. Korr “spent decades adding scientific legitimacy, through experimentation and publication, to the clinically based practice of osteopathy. Much of their earlier work center on demonstrating the hyperarousal of the sympathetic nervous system associated with what was then termed the osteopathic lesion.”
Dr. Korr has 51 articles in a PubMed search of the US National Library of Medicine, spanning the years 1946-2002. Decades of Dr. Korr’s research, experimentation and publications are summarized in his 1979 article titled (6):
The spinal cord as organizer of disease processes:
Hyperactivity of sympathetic innervation as a common factor is disease
Dr. Korr reviews the evidence showing that somatic musculoskeletal problems, especially increased muscle tone that reduce motion and create stiffness, influence the sympathetic nervous system. In summary, spinal stiffness caused sympathetic excitation, vasoconstriction, and therefore reduced blood delivery. The region of spinal stiffness would determine the region of sympathetic excitation and vasoconstriction.
••••
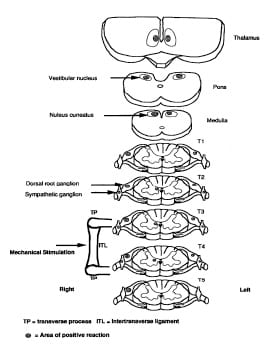
Dr. Korr’s physiological explanations were enhanced significantly in 1997 with the work of Hongxing Jiang, PhD, and colleagues from the Department of Surgery, University of Alberta, Edmonton, Canada. Their article was published in the journal Spine, and titled (7):
Identification of the Location, Extent, and Pathway of Sensory Neurologic Feedback After Mechanical Stimulation of a Lateral Spinal Ligament in Chickens
By immunohistochemically locating the sites of Fos protein production in neuronal cell bodies, Dr. Jiang and colleagues were able to trace the location, extent, and pathways of sensory feedback after the mechanical stretching of a lateral spinal ligament. The presence of Fos indicated the physiological neurological chain cascade that was initiated by a mechanical input into a single spinal ligament.
The results showed that a mechanical input to the intertransverse ligament would stimulate the following sequence of neurons:
- The dorsal root ganglia at the level of stimulation, at the level above stimulation, and at the level below stimulation (therefore at 3 levels). This shows that a carefully applied mechanical sensory input enters the spinal cord a three adjacent spinal levels.
- The intermediate gray matter of the spinal cord at the level of stimulation as well as the spinal cord level above and below the site of stimulation. This is quite important. The intermediate gray matter of the spinal cord is located in the seventh layer of the spinal grey matter (lamina VII). It is also known that the second order neuron for mechanical afferentation has cell bodies in the seventh layer of the spinal grey matter (lamina VII), so this finding makes logical sense. It also known that the pre-ganglionic neurons of the sympathetic branch of the autonomic nervous system are located in the intermediate gray matter of the spinal cord.
- The sympathetic chain ganglia, once again at the level of stimulation as well as the spinal cord level above and below the site of stimulation. This is most important because is confirms the writings of Dr. Korr, confirming that there is a communication between spinal mechanical function and the sympathetic nervous system. This concept is used below as a physiological influence on brain function (9).
- The combined nucleus cuneatus and gracilis in the medulla oblongata. This indicates that spinal mechanical function influences the brainstem.
- The vestibular nuclei, also of the medulla oblongata. This indicates that spinal mechanical function also influences balance and muscle tone.
- The thalamus. This is very important to this discussion as the thalamus is in the brain. The thalamus is the pre-synaptic integrated pool of neurons that control much of brain cortical function. The authors did not assess brain cortical Fos production, a shortcoming that they self-criticize.
Dr. Jiang and colleagues note that spinal ligaments are not “simple mechanical constraints across joints that provide tension when stretched.” Additional functional roles for spinal ligaments include the coordination of muscle tone around joints and to provide a neurologic feedback mechanism to enhance joint stability. They state:
“In light of these results it is now thought that ligaments do more than act as simple mechanical links between bones; they also may provide important proprioceptive feedback as part of a neurologic protective mechanism for the ligaments themselves and for the joints they span.”
In this study, Dr. Jiang and colleagues note that spinal ligaments are richly innervated with mechanoreceptors and nociceptors. The mechanoreceptors function as initiators of feedback pathways that include the spine, the brain stem, the brain and the sympathetic nervous system. These authors state:
“The results of the current study have shown that mechanical stretching of an important lateral spinal ligament in chickens produced a barrage of sensory feedback from several levels of the spinal cord and responses from the contralateral side of the cord at equivalent levels. Further, the pathway of the sensory input can be traced to include nerve cell bodies in the dorsal root ganglia, the sympathetic ganglia, the intermediate horn of the spinal cord, the cuneatus and gracilis nuclei of the medulla oblongata, the vestibular nuclei, and the thalamus.”
From Jaing, (7):
••••
Dr. Korr’s work was further enhanced in 2007 with the work of Heidi Haavik-Taylor and Bernadette Murphy from the University of Auckland. New Zealand. Published in the journal Clinical Neurophysiology and titled (8):
Cervical spine manipulation alters sensorimotor integration:
A somatosensory evoked potential study
Drs. Haavik-Taylor and Murphy recorded the neurophysiological effects of cervical spine manipulation to dysfunctional cervical joints using brainstem and cortical somatosensory evoked potentials (SEPs) in 12 subjects. They also recorded these electrical signals in a control group (also 12 subjects) who were passively mobilized but not manipulated.
Results show a significant change in the amplitude of parietal (sensory) and frontal (motor) SEP components following the single session of cervical spine manipulation. No SEP changes were observed in the passive head movement control condition. The authors state:
“This study suggests that cervical spine manipulation may alter cortical somatosensory processing and sensorimotor integration.”
“These findings may help to elucidate the mechanisms responsible for the effective relief of pain and restoration of functional ability documented following spinal manipulation treatment.”
“The passive head movement SEP experiment demonstrated that no significant changes occurred following a simple movement of the subject’s head. Our results are therefore not simply due to altered input from vestibular, muscle or cutaneous afferents as a result of the chiropractor’s touch or due to the actual movement of the subjects head. This therefore suggests that the results in this study are specific to the delivery of the high-velocity, low-amplitude thrust to dysfunctional joints.”
“Spinal manipulation of dysfunctional joints may modify transmission of neuronal circuitries not only at a spinal level but at a cortical level, and possibly also deeper brain structures such as the basal ganglia.”
The spinal manipulation in this study was applied to dysfunctional cervical joints, as determined by a “registered chiropractor.”
The clinical evidence for joint dysfunction includes:
- Tenderness on joint palpation.
- Restricted intersegmental range of motion.
- Palpable asymmetry of intervertebral muscle tension.
- Abnormal or blocked joint play and end-feel.
- Sensorimotor changes in the upper extremity.
“The most reliable spinal dysfunction indicator is tenderness with palpation of the dysfunctional joint.” To assess joint dysfunction, cervical range of motion also has good reliability. Therefore, in this study, cervical spinal dysfunction was defined as having both restricted intersegmental range of motion and tenderness to palpation of the restricted joint.
This study documents cortical brain changes as a consequence of cervical spinal adjusting.
••••
Late last year (December 2011), a study was published in the PubMed indexed journal Alternative Therapies Health Medicine, titled (9):
Cerebral metabolic changes in men
after chiropractic spinal manipulation for neck pain
The authors are from the Division of Cyclotron Nuclear Medicine, Tohoku University (Graduate School of Medicine), Sendai, Japan. I believe that their work integrates that of Korr, Jiang, and Haavik-Taylor/Murphy.
The authors cite 9 studies that have found that spinal dysfunction affects the autonomic nervous system. This is in agreement with the studies of Korr (6) and Jiang (7). They note that the sympathetic branch of the autonomic nervous system controls the diameter of the arterial system. Increased sympathetic tone would cause vasoconstriction, reducing the delivery of glucose and thereby reducing the uptake metabolism of glucose into ATP energy.
Consequently, the authors created a radioactive analog of glucose (FDG = 18F-labeled flurodeoxyglucose), which is an excellent imaging marker of brain glucose consumption (brain metabolic activity).
Positron emission tomography (PET) scan is a powerful neuroimaging technique to investigate neuronal activity in the human brain, including the uptake of glucose for metabolism. Using PET and FDG, the authors evaluated brain regions in 12 men before and after chiropractic spinal adjusting. This is the first chiropractic study to examine regional cerebral metabolism using positron emission tomography (PET).
Results from this study include:
- Questionnaires indicated lower stress levels and better quality of life following chiropractic spinal manipulation.
- A significantly lower visual analog scale (VAS) was noted after chiropractic spinal manipulation.
- Cervical muscle tone decreased after chiropractic spinal manipulation.
- Salivary amylase was decreased after chiropractic spinal manipulation. Salivary amylase is a marker for sympathetic tone; consequently, sympathetic tone was decreased after chiropractic spinal manipulation.
The authors concluded that the spinal adjustment improved mechanical function, reduced neck pain, inhibited the sympathetic nervous system, improved brain blood flow, enhanced brain glucose utilization, improving brain function. Importantly for this discussion, the authors clearly document improved brain function in the limbic system. These authors state:
“The results of this study suggest that CSM affects regional cerebral glucose metabolism related to sympathetic relaxation [inhibition] and pain reduction.”
“In summary, the present study demonstrated sympathetic relaxation [inhibition] and corresponding regional brain metabolic changes, as well as reduced muscle tone and decreased pain intensity following a chiropractic spinal manipulation.”
The chart below summarize their findings:
Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain
| Assessment | After Chiropractic Spinal Adjustment | Interpretation |
| Stress Response Scale = SRS-18 | “Significantly Lower” | Significantly reduced stress secondary to sympathetic inhibition |
| EORTC QLQ-C30 | “Significantly Lower” | Significantly improved quality of life |
| Visual Analog Scale = VAS | “Significantly Improved”
[reduced] |
Significantly reduced stress secondary to sympathetic inhibition |
| Cervical (Trapezius) Muscle Tone | “Significantly Improved”
[reduced] |
Secondary to sympathetic inhibition
(Hubbard study, Spine, 1993) |
| Salivary Amylase | “Significant Decrease” | Secondary to sympathetic inhibition |
| Inferior Prefrontal Cortex | Increased Glucose Metabolism | Secondary to sympathetic inhibition |
| Middle Temporal Gyrus
[limbic system] |
Increased Glucose Metabolism | Secondary to sympathetic inhibition |
| Anterior Cingulate Cortex
[limbic system] |
Increased Glucose Metabolism | Secondary to sympathetic inhibition |
| Cerebellar Vermis | Decreased Glucose Metabolism | [Secondary to improved midline spinal mechanical afferentation] |
Summary and Proposed Model
Chiropractors frequently observe and therefore talk about the improvement of non-musculoskeletal syndromes, including brain function, in patients under chiropractic care. A number of lines of scientific investigations make the following mechanism biologically plausible:
The spinal adjustment is intended to improve the way the patient lives, functions, and exists in a gravity environment. The improvement in spinal mechanical function “closes the pain gate,” and pain perception is reduced (inhibited). (10)
The spinal adjustment improves the function of spinal mechanoreceptors. These spinal mechanoreceptors are proven to exist in the annulus of the intervertebral disc (11, 12), the facet joint capsules (13, 14), the supraspinous/interspinous ligaments (15), and the muscle spindles (16, 17).
Spinal mechanoreceptors are proven to communicate with the sympathetic nervous system (preganglionic sympathetic efferents in lamina VII of the spinal cord), and their influence is inhibitory (18, 19).
The sympathetic neurons innervate the blood vessels, including those in the brain. Increased sympathetic tone causes vasoconstriction, reducing the delivery of blood and therefore of glucose and oxygen, and thereby reducing the production of ATP energy. Brain function is dependent upon the production of ATP energy (20).
Chiropractic spinal adjusting appears to influence brain function primarily in two ways:
- Direct alterations of brain electrical signals.
- Inhibition of the sympathetic nervous system, subsequent vasodilation, improved glucose delivery to brain neurons resulting in increased uptake and energy synthesis.
Spinal adjusting works in part because of inhibition of increased sympathetic tone.
The studies presented here support a link between spinal function, chiropractic spinal adjusting, and limbic emotional function. They may help explain the anecdotal observations of the Kentucky House of Reform and North Dakota’s Judge Ponath.
In today’s modern environment, few chiropractors would treat patients for brain dysfunction alone. Yet, many chiropractors treat patients with brain dysfunction, along with other qualified providers. Even the publication from the Kentucky House of Reform in 1931 clearly noted that the chiropractors were a part of a team of medical providers, and that the chiropractor enhanced the clinical outcome, helping the patient, the patient’s family, and the taxpayers. Many patients with a variety of brain disorders could benefit from the chiropractic improvement of their spinal mechanical function.
REFERENCES:
- Cyriax J; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions, eighth edition; Bailliere Tindall, 1982.
- Marshall LT; REPORT: State Supervisor of Chiropractic; In Connection with Kentucky House of Reform; 1931.
- Ponath AW; FACTS: What Chiropractic has done for Insanity; 1934.
- The American Physiological Society; http://www.the-aps.org/MayCC/membership/obituaries/irvinkorr.txt
- Chaitow L, Comeaus Z, Liebenson C; Obituary: Irvin Korr Ph.D. (1909-2004); 8, pp. 155-157.
- Korr IM; The spinal cord as organizer of disease processes: Hyperactivity of sympathetic innervation as a common factor is disease; Journal of the American Osteopath Association; 1979 Dec;79(4):232-7.
- Jiang H, Moreau M, Raso M, Russell G, Bagnall K; Identification of the Location, Extent, and Pathway of Sensory Neurologic Feedback After Mechanical Stimulation of a Lateral Spinal Ligament in Chickens; SPINE 1997;22:17-25 (January 1, 1997).
- Haavik-Taylor H, Murphy B; Cervical spine manipulation alters sensorimotor integration: A somatosensory evoked potential study; Clinical Neurophysiology; February 2007 Feb;118(2):391-402.
- Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, Itoh M, Fukuda H, Yanai K; Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain; Alternative Therapies Health Medicine; Nov-Dec 2011;Vol. 17; No. 6; pp. 12-7.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985, Vol. 31, pp. 535-540.
- Mendel T, Wink CS, Zimny ML; Neural elements in human cervical intervertebral discs; Spine (Phila Pa 1976). 1992 Feb;17(2):132-5.
- Roberts S, Eisenstein SM, Menage J, Evans EH, Ashton IK; Mechanoreceptors in intervertebral discs. Morphology, distribution, and neuropeptides; Spine (Phila Pa 1976). 1995 Dec 15;20(24):2645-51.
- McLain RF; Mechanoreceptors endings in human cervical facet joints; Spine (Phila Pa 1976). 1994 Mar 1;19(5):495-501.
- McLain RF; Pickar JG; Mechanoreceptor Endings in Human Thoracic and Lumbar Facet Joints; SPINE 1998;23:168-173.
- Jiang H, Russell G, Raso J, Marc J. Moreau MJ, Hill DL, Bagnall KM; The Nature and Distribution of the Innervation of Human Supraspinal and Interspinal Ligaments; SPINE Volume 20, Number 8, pp. 869-876 (April 15, 1995).
- Solomonow M, Zhou BE Harris, Lu MY, Baratta RV; The Ligamento-Muscular Stabilizing System of the Spine; SPINE: Dec 1, 1998;23:2552-2562.
- Holm S, Indahl A, Solomonow M; Sensorimotor control of the spine; Journal of Electromyography and Kinesiology; Volume 12, Issue 3, June 2002, pp. 219-234.
- Budgell B, Hirano F; Innocuous mechanical stimulation of the neck and alterations in heart-rate variability in healthy young adults; Autonomic Neuroscience. 2001 Aug 13;91(1-2):96-9.
- Koch LE, Koch H, Graumann-Brunt S, Stolle D, Ramirez JM, Saternus KS; Heart rate changes in response to mild mechanical irritation of the high cervical spinal cord region in infants; Forensic Science International; Volume 128, Issue 3, August 28, 2002, Pages 168-176.
- Perlmutter D; The Better Brain Book; Riverhead Books, 2004, pp. 21-23.