The total sum of suffering caused by migraine headache is higher than any other kind of headache (1). About 38 million adults in the United States are migraine sufferers, and 91% experience migraine-associated disability (2, 3, 4).
Migraine headache is often incapacitating, with considerable impact on social activities and work, and may lead to significant consumption of drugs (1). Commonly prescribed rescue medications (analgesics, ergots, triptans, and opioids) may increase the risk of medication overuse headaches, allodynia, and dependence (5).
An article appearing in the Business Section of the San Francisco Chronicle newspaper on July 20, 2014, notes that the migraine market in developed countries will grow to about $5.4 billion in 2022 (6). The author, Stephanie Lee, notes that current treatments are not very effective and they may have dangerous side effects:
“Frustrated patients often seek out opioids in the emergency room, but opioids can be dangerous. In a year, … 20,000 patients in California developed chronic migraines because of opioid overuse, and 3,000 became addicted.”
It is ironic that opioids taken for migraines cause chronic migraines in many patients. Ms. Lee concludes (6):
“The demand for safe and effective alternatives [for migraine headaches] is urgent.”
Approximately 40% of those with episodic migraines have unmet treatment needs, including dissatisfaction with treatment and moderate or severe headache-related disability (7). Evidence is mounting, (presented here), that chiropractic and spinal manipulation may provide a sought-after safe and effective alternative to pharmacology and reduce the incidence of unmet treatment needs.
••••••••••
Perhaps his most important contribution to the understanding of the clinical anatomy of headache, including migraine headache, appeared in the journal Biomedicine and Pharmacotherapy in 1995. The article is titled (8):
Anatomy and Physiology of Headache
In this article, Dr. Nikolai Bogduk notes that “all headaches have a common anatomy and physiology,” including migraine headache. They are all “mediated by the trigeminocervical nucleus.” The trigeminocervical nucleus is located at the upper aspect of the neck. Consequently, all headaches, including migraine headaches, synapse in the upper aspect of the neck. Anatomically, this presents a potential mechanism by which upper neck manipulation could have an influence on migraine headaches.
The trigeminocervical nucleus is “defined by its afferent fibers.” The primary afferent fibers to the nucleus are from the Trigeminal Nerve (Cranial Nerve V), and from the upper three cervical nerves (C1, C2, C3). All headaches synapse in the trigeminocervical nucleus. Second order afferent neurons arising in the trigeminocervical nucleus ascend to create an electrical signal in the brain that is interpreted as “headache.”
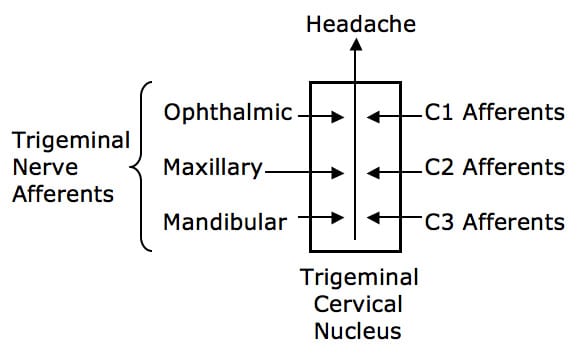
Upper cervical spine afferents may be a source of the electrical signal that is interpreted as headache in the brain, including migraine headache. Consequently, structures that are innervated by C1, C2, and C3, can cause headaches, including migraine, when irritated and/or inflamed.
Review of Recent Clinical Studies
In 1978, an early study was published in the Australian and New Zealand Journal of Medicine titled (9):
A Controlled Trial of Cervical Manipulation of Migraine
The efficacy of cervical manipulation for migraine was evaluated in a six-month trial using 85 migraine sufferers. The cervical manipulation was randomly performed by a medical practitioner, a physiotherapist, or chiropractor. The authors stated:
“For the whole sample, migraine symptoms were significantly reduced.”
“Chiropractic patients did report a greater reduction in pain associated with their attacks.”
•••••
In 2000, a study was published in the Journal of Manipulative and Physiological Therapeutics titled (10):
A Randomized Controlled Trial of
Chiropractic Spinal Manipulative Therapy for Migraine
This randomized controlled trial was of 6 months duration. It used 127 subjects. The outcome measures used included frequency, intensity (visual analogue score), duration, disability, and use of medication for each.
The chiropractic manipulation treatment group “showed statistically significant improvement in migraine frequency, duration, disability, and medication use when compared with the control group.”
“Twenty-two percent of participants reported more than a 90% reduction of migraines as a consequence of the 2 months of spinal manipulative therapy.”
“The results of this study support previous results showing that some people report significant improvement in migraines after chiropractic spinal manipulative therapy.”
In June 2014, a study was published in the journal Headache, titled (11):
Cervical Referral of Head Pain in Migraineurs:
Effects on the Nociceptive Blink Reflex
This study assessed the pain intensity and nociceptive blink reflex in 15 migraine subjects between times of symptoms with passive movements of the occipital and upper cervical spinal segments. The authors note that anatomically and neurophysiologically there is a functional convergence (see above drawing) of trigeminal and cervical afferent pathways.
This study showed that passive manual intervertebral movement between the occiput and the upper cervical spinal joints decreases excitability of the trigeminocervical nucleus. They note that manual cervical modulation of this pathway is of potential benefit in migraine sufferers. The authors concluded:
Ongoing noxious sensory input arises from biomechanically dysfunctional spinal joints. Mechanoreceptors including proprioceptors (muscle spindles) within deep paraspinal tissues react to mechanical deformation of these tissues. Manual mechanical deformation can cause “biomechanical remodeling” with restoration of zygapophyseal joint mobility and joint “play.” “Biomechanical remodeling resulting from mobilization may have physiological ramifications, ultimately reducing nociceptive input from receptive nerve endings in innervated paraspinal tissues.”
These findings “corroborate previous results related to anatomical and functional convergence of trigeminal and cervical afferent pathways in animals and humans, and suggest that manual modulation of the cervical pathway is of potential benefit in migraine.”
This article supports the clinical anatomical perspective of Dr. Bogduk. It also supports the concept for the inclusion of manual/manipulative therapy of the upper cervical spine in the management of migraine headaches.
•••••
In 2015, the journal Complementary Therapies in Medicine, published a study titled (12):
Clinical Effectiveness of Osteopathic Treatment in Chronic Migraine:
3-Armed Randomized Controlled Trial
The authors of this study note that this manipulative therapy trial is the largest ever conducted on adult migraine patients. The authors assessed the effectiveness of manipulative treatment on 105 chronic migraine patients.
The authors note that manipulation in migraine could reduce the release of pro-inflammatory substances that have an effect on the nociceptive nervous system. Key findings from this study include:
- At the end of the study period, the manipulation group was statistically improved from the control and sham group.
- Manipulation “significantly reduced the frequency of migraine.”
- Manipulation “significantly reduced the number of subjects taking medications.”
- Manipulation “showed a significant improvement in the migraineurs’ quality of life.”
- No study participant reported any adverse effects of the manipulation.
- The use of manipulative therapy as an “adjuvant therapy for migraine patients may reduce the use of drugs and optimize the clinical management of the patients.”
- Manipulation “may be considered a clinically valid procedure for the management of patients with migraine.”
•••••
In 2017, researchers from Akershus University Hospital, Oslo, Norway, and the Department of Chiropractic, Macquarie University, NSW, Australia, published a study in the journal Musculoskeletal Science and Practice titled (13):
Adverse Events in a Chiropractic Spinal Manipulative Therapy:
Single-blinded, Placebo, Randomized Controlled Trial for Migraineurs
The primary objective of this study was to report on all adverse events in a prospective chiropractic spinal manipulative therapy, single-blinded, placebo, randomized controlled trial for migraineurs.
The authors note that migraines are a common worldwide challenge, and pharmacological management is often the first treatment of choice. However, migraine drugs can have serious and/or undesirable side effects. In contrast, manual-therapy is a non-pharmacological migraine treatment option that appears to have a similar effect as common drugs on migraine frequency, migraine duration, and migraine intensity.
This study prospectively reported all adverse events in a chiropractic spinal manipulative therapy randomized controlled trial. It is a prospective assessment; 70 migraineurs were randomized to chiropractic manipulation (Gonstead full-spine adjusting) or a placebo, with 12 intervention sessions over three months. The Gonstead chiropractic spinal adjusting method is a specific contact, high-velocity, low-amplitude, short-lever spinal manipulation directed to spinal biomechanical dysfunction.
The subjects attended 12 intervention sessions over 12 weeks with follow-up at 3, 6, and 12-months post-treatment. The authors concluded:
This study “showed significant differences between the chiropractic spinal manipulation group and the control group [drug group] at all post-treatment time points.”
“Adverse events in migraine prophylactic pharmacological randomized clinical trials are common. The risk for adverse events during manual-therapy [is] substantially lower than the risk accepted in any medical context for both acute and prophylactic migraine medication.”
Non-pharmacological management of migraines has the advantage of having mild and transient adverse events, “whereas pharmacological adverse events tend to be continuous.”
“Chiropractic spinal manipulation applying the Gonstead technique appears to be safe for the management of migraine headache and presents few mild and transient adverse events.”
In this study, Gonstead chiropractic adjusting had the best long-term clinical results.
•••••
In 2019, a study was published in the journal Headache, titled (14):
The Impact of Spinal Manipulation on Migraine Pain and Disability:
A Systematic Review and Meta-Analysis
This study is a systematic review and meta-analysis of published randomized clinical trials to evaluate the evidence regarding spinal manipulation as an alternative or integrative therapy in reducing migraine pain and disability. The authors identified 6 randomized clinical trials eligible for their analysis that included 677 subjects. The spinal manipulations were performed by a chiropractor in 3 studies, an osteopath in 2 studies, and undetermined in 1 study.
The intervention duration ranged from 2 to 6 months, and the number of treatments ranged from 8 to 16. Outcomes included number of migraine days (primary outcome), migraine pain/intensity, and migraine disability.
The authors include a discussion pertaining to problems with pharmacology for migraine headaches and the need for non-drug approaches to the migraine issue. They note:
“The limitations to current pharmacological therapies have highlighted the need to explore alternative or integrative treatments for migraine.”
There is a need for evidence-based non-pharmacological approaches to treat migraines, and to “understand whether spinal manipulation, an integral component to chiropractic care, is an effective non-pharmacological approach for the treatment of migraine headaches.”
“Spinal manipulation may be an effective therapeutic technique to reduce migraine days and pain/intensity.”
“One potential non-pharmacological approach to the treatment of migraine patients is spinal manipulation, a manual therapy technique most commonly used by doctors of chiropractic.”
Pertaining to chiropractic and spinal manipulation, the authors note that 94% of spinal manipulation for which reimbursement is sought in the United States is delivered by chiropractors, and:
“In the United States, approximately 12% of patients seeking treatment from a chiropractor report headache as their chief complaint.”
Approximately 15.4% of individuals with migraines have used chiropractic care in the past 12 months.
Fifty three percent of chiropractors reported managing patients with migraines “often.”
Forty one percent of chiropractors reported managing patients with migraines “sometimes.”
The conclusion of this meta-analysis is that spinal manipulation had a greater impact on reducing the number of migraine days compared to controls. The authors state:
“In this meta-analysis, spinal manipulation was associated with significant reductions in migraine days compared to those in active control groups which suggests that the results seen for the intervention group are not solely due to attention or expectation.”
“Results from this preliminary meta-analysis suggest that spinal manipulation may reduce migraine days and pain/intensity.”
Importantly, the authors note that their review focused on spinal manipulation, yet they acknowledged that chiropractic clinical practice often uses a multimodal approach which may also be beneficial, including but not limited to education, spinal stabilization exercises, soft tissue manipulation, breathing training, stretching techniques, nutrition, and ergonomic modifications.
The authors also address the issue of potential adverse events that might arise from cervical spine manipulation. They were particularly mindful of cervical artery dissection because of concerns that cervical manipulation may be associated with cervical artery dissection and because there is an increased risk of cervical artery dissection among migraineurs. The authors found:
“Few adverse events were observed and none were considered serious or severe.”
•••••
Lastly, and importantly, this same group published a study in the journal Global Advances in Health and Medicine in March 2019, titled (15):
Integrating Chiropractic Care into the Treatment of
Migraine Headaches in a Tertiary Care Hospital: A Case Series
These authors are from Brigham and Women’s Hospital, Boston, and Harvard Medical School. They are specifically including chiropractic in the treatment of migraine headache. They state:
In the past decade, there has been a “rise in the number of chiropractors working collaboratively with medical practitioners and many are integrated into medical facilities, including at the Harvard Medical School Osher Center for Integrative Medicine.”
“Many medical practitioners are often unaware of the treatment approaches within the chiropractic profession and the efficacy of these approaches because chiropractors have practiced as a separate health-care system for over a century.”
“This article serves to inform medical colleagues of the scope and depth of chiropractic training and treatment and how integration of care might be beneficial to a neurology practice.”
The rationale for using chiropractic care for these migraine patients includes these points:
- Migraines “can be managed, but there is no cure, and many medications used to treat migraines have disabling side effects.”
- “Patients often prefer to avoid daily medication and seek nonpharmacologic options, including complementary and integrative therapies.”
- In 2007, the Harvard Medical School Osher Center for Integrative Medicine established the Osher Clinical Center for Complementary and Integrative Therapies based at Brigham and Women’s Hospital. A central focus of the Osher Clinical Center is treatment of musculoskeletal pain, and the “most widely used modality is chiropractic.”
- “Our patients have expressed the desire for integrated models of care, particularly to minimize medication use.”
- “Over 75% of migraine patients report associated neck pain, and many note musculoskeletal complaints, such as neck stiffness, muscle tension, or problems with jaw function.”
- “Typical allopathic treatments for such neck pain include muscle relaxants, nonsteroidal anti-inflammatory drugs, and physical therapy, but these are often inadequate in addressing the underlying dynamics of these complaints and individuals with migraines frequently report unmet treatment needs.”
Chiropractors are licensed to administer nonsurgical and nonpharmacological therapies for health restoration and maintenance. The chiropractic approach to patients suffering migraine headaches may include combinations of spinal manipulative therapy, soft tissue therapies (myofascial release, massage, trigger point therapies, etc.), rehabilitation/exercises, ergonomic advice, lifestyle management, and nutritional counseling. Chiropractic has “been shown to be efficacious for a wide-range of musculoskeletal conditions including neck pain and temporomandibular pain.” The goals of chiropractic therapy are to optimize neuromusculoskeletal health and reduce the patient’s overall pain burden.
The authors present a three migraine patient case series that illustrates an integrated model of care for migraine patients that combines standard neurological care with chiropractic treatment. Each patient initially presented to a neurologist and was subsequently referred to a chiropractic colleague. A summary of the presented cases follows:
Case 1:
42-year old female with migraine headaches 3 to 4 times weekly.
She also had temporomandibular joint pain and neck pain.
With chiropractic care, including spinal manipulation, there was a “nearly immediate reduction in headache and neck pain and a reduced headache frequency to 1 per month.”
Case 2:
34-year old female with daily migraines for 12 years 7-8/10 intensity.
Multiple medications provided limited relief.
After 9 months of chiropractic, headaches reduced to 10 per month with average pain rating of 3/10. At 10 months, she experienced her first headache free month.
Case 3:
29-year old female with migraines nearly daily for 16 years.
There was a near immediate positive response to chiropractic care in headache and neck pain intensity and frequency. There was a 50% reduction in headache intensity.
Findings from the 3 presented case studies integrating neurologic and chiropractic care for the treatment of migraine included:
- Improvement in pain scores
- Increase in pain-free days
- Decreased medication usage
- Patient reported decreased anxiety/dysthymia
The authors state the most promising migraine patient candidates for integration of chiropractic care include:
- Patients seeking non-drug approaches or wanting to reduce drug usage.
- Nonresponsive patients in need of concurrent multipronged care.
- Patients who have reached a therapeutic plateau in need of sequential care.
The authors stated:
“All patients reported greater therapeutic benefits with the addition of the integrative approach.”
“Our case series highlights the promise of and the need to further evaluate integrated models of chiropractic and neurologic care.”
Summary
These studies document what essentially every chiropractor has observed for more than a century:
Improvement of the mechanical function of the upper cervical spine with spinal manipulation and other adjunctive mechanical interventions is effective and safe intervention for patients suffering from migraine headache.
The benefits of chiropractic spinal manipulation is not only that it is effective and safe, but that it helps patients avoid problems associated with pharmacological treatment.
REFERENCES
- Olsen J, Tfelt-Hansen P, Welch KMA; The Headaches, second edition; Lippincott Williams & Wilkins; 2000.
- Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML; Burden of migraine in the United States: Disability and economic costs; Archives of Intern Medicine; April 26, 1999; Vol. 159; No. 8; pp.813-818.
- Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M; Prevalence and burden of migraine in the United States: Data from the American Migraine Study II; Headache; July-August 2001; Vol. 41; No. 7; pp. 646-657.
- Lipton RB, Bigal ME, Diamond M, et al.; Migraine prevalence, disease burden, and the need for preventive therapy; Neurology; January 30, 2007; Vol. 68; No. 5; pp. 343-349.
- Thorlund K, Sun-Edelstein C, Druyts E, et al.; Risk of medication overuse headache across classes of treatments for acute migraine; Journal of Headache Pain; December 2016; Vol. 17; No. 1; p. 107.
- Lee, SM; Huge Headache of a Problem; Mastering Migraines Still a Challenge for Patients, Scientists; San Francisco Chronicle; July 20, 2014; pp. D1 and D5.
- Lipton RB, Buse DC, Serrano D, Holland S, Reed ML; Examination of unmet treatment needs among persons with episodic migraine: Results of the American Migraine Prevalence and Prevention (AMPP) study; Headache; September 2013; Vol. 53; No. 8; pp. 1300-1311.
Bogduk N; Anatomy and Physiology of Headache; Biomedicine and Pharmacotherapy; 1995; Vol. 49; No. 10; pp. 435-445. - Parker GB, Tupling H, Pryor DS; A controlled trial of cervical manipulation of migraine; Australian and New Zealand Journal of Medicine; December 1978; Vol. 8; No. 6; pp. 589-593.
- Tuchin PJ, Pollard H, Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine; Journal of Manipulative and Physiological Therapeutics; 2000; Vol. 23; pp. 91-95.
- Watson DH, Drummond PD; Cervical Referral of Head Pain in Migraineurs: Effects on the Nociceptive Blink Reflex; Headache 2014; Vol. 54; pp. 1035-1045.
- Cerritelli F, Ginevri L, Messi G, Caprari E, Di Vincenzo M, Renzetti C, Cozzolino V, Barlafante G, Foschi N, Provincial L; Clinical Effectiveness of Osteopathic Treatment in Chronic Migraine: 3-Armed Randomized Controlled Trial; Complementary Therapies in Medicine; April 2015; Vol. 23; No. 2; pp. 149—156.
- Chaibi A, Benth JS, Tuchin PJ, Russell MB; Adverse Events in a Chiropractic Spinal Manipulative Therapy Single-blinded, Placebo, Randomized Controlled Trial for Migraineurs; Musculoskeletal Science and Practice; March 2017; Vol. 29; pp. 66-71.
- Rist PM, Hernandez A, Bernstein C, Kowalski M, Osypiuk K, Vining R, Long CR, Goertz C, Song R, Wayne PM; The Impact of Spinal Manipulation on Migraine Pain and Disability: A Systematic Review and Meta-Analysis; Headache; April 2019; Vol. 59; No. 4; pp. 532-542.
- Bernstein C, Wayne PM, Rist PM, Osypiuk K, Hernandez A, Kowalski M; Integrating Chiropractic Care into the Treatment of Migraine Headaches in a Tertiary Care Hospital: A Case Series; Global Advances in Health and Medicine; March 28, 2019; [epub]
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”
