Perhaps the most authoritative book written pertaining to the spine is Schmorl’s and Junghanns’ The Human Spine in Health and Disease. Georg Schmorl (1861-1932) was a German physician and pathologist. Herbert Junghanns (1902-1986) was the Chief of the Occupational Accident Hospital, Surgical Clinic, and Head of the Institute for Spinal Column Research, in Frankfurt, Germany. The first edition of their book was published in 1932, shortly before the death of Dr. Schmorl. The fifth German edition of their book was translated into English in 1971 (1). This incredible book contains 500 figures of radiographs, histological sections, photographs, and drawings. The book has more than 500 pages and approximately 5,000 references in the bibliography.
In their book, Drs. Schmorl and Junghanns note:
“Like other body articulations, the apophyseal joints are endowed with articular capsules, reinforcing ligaments and menisci-like internal articular discs.” p. 251
“Like any other joint, the motor segment may become locked. This is usually associated with pain.” Chiropractors refer to such events as subluxations. These motor unit disturbances can cause torticollis and lumbago. “Various processes may cause such ‘vertebral locking.’ It may happen during normal movement. The incarceration of an articular villus or of a meniscus in an apophyseal joint may produce locking.” pp. 221-222
If a joint is suddenly incarcerated within the range of its physiologic mobility, as occurs with the meniscus incarceration of the knee joint, it is an “articular locking or a fixed articular block.”
“Such articular locking is also possible in the spinal articulations (apophyseal joints, intervertebral discs, skull articulations, lumbosacral articulations). They may be mobilized again by specific therapeutic methods (stretchings, repositioning, exercises, etc.). Despite many opinions to the contrary, this type of locking is today increasingly recognized by physicians. Many physicians are employing manipulations which during the past decades were the tools of lay therapists only (chiropractors, osteopaths). However, these methods have at times been recommended by physicians. They have also been known in folk medicine and in medical schools of antiquity.” p. 376
Accompanying these quotes and other pertinent discussions are two photographs of anatomical sections through the facet joints showing these “menisci-like internal articular discs,” or meniscus. They also included three radiographs and one drawing showing abnormal gapping of an articulation as a consequence of meniscus entrapment in a facetal articulation. They note that such a meniscoid incarceration can cause acute torticollis, and they show a “follow-up roentgenogram after manual repositioning” resulting in “immediate relief of complaints and complete mobility.” p. 222
In September 1975, the Department of Physical Medicine and Rehabilitation of the California College of Medicine organized an international conference concerning Approaches to the Validation of Manipulation Therapy. The conference was held at the University of California, Irvine. Twenty-one global top experts on spinal manipulation participated in the conference. The proceedings from the conference were published in 1977, edited by Alfred Buerger, PhD, and Jerome Tobis, MD. Dr. Buerger was an assistant professor from the Department of Physical Medicine & Rehabilitation and Physiology at the medical school at the University of California Irvine, and Dr. Tobis was a Professor and Chairman of the Department of Physical Medicine and Rehabilitation of the medical school at the University of California Irvine (2). Chapter 14 of the conference proceedings was authored by physician James Fisk from New Zealand (3). The title of Dr. Fisk’s chapter 14 is:
An Evaluation of Manipulation in the Treatment of the Acute Low Back Pain Syndrome in General Practice
In this chapter, Dr. Fisk, in the section regarding possible lesions that cause low back pain, lists:
“Entrapment of a Meniscoid”
“These meniscoids are richly innervated by pain producing nerve endings. There should be a rapid response to manipulation.”
In 1977, the National Institute of Neurological and Communicative Disorders and Stroke of the National Institutes of Health (USA), funded a grant for a Research Workshop on Neurobiologic Mechanisms in Manipulative Therapy. The workshop was held at Michigan State University, and had 38 worldwide participant experts. The Proceedings for the workshop were published the following year (4), 1978, edited by Irvin Korr, Professor from the Department of Biomechanics, College of Osteopathic Medicine, Michigan State University. The first chapter of the workshop proceedings is authored by Dr. Karel Lewit from Czechoslovakia, and is titled (5):
The Contribution of Clinical Observation to
Neurobiological Mechanisms in Manipulative Therapy
In this chapter, Dr. Lewit notes:
“The meniscoid has a soft base and a hard edge.”
“If the meniscoid is caught between the gliding surfaces of the joint facets the hard edge produces a cavity in the cartilage in which it is trapped.”
“The implications for the theory of manipulation are obvious: if we separate the joint facets the meniscoid can slip out.”
Dr. Lewit includes a similar discussion in his 1985 text titled Manipulative Therapy in Rehabilitation of the Locomotor System (6).
Also in 1985, 30 distinguished international multidisciplinary experts collaborated on a text titled Aspects of Manipulative Therapy (7). The comments in this text pertaining to the interarticular meniscus include:
“Histologically, meniscoids are synovial tissue.”
“Their innervation is derived from that of the capsule.”
The current hypothetical model of the mechanism involved in acute joint locking is based on a phenomenon in which the “meniscoid embeds itself, thereby impeding mobility.”
“It is highly probable that the meniscoids do play an important role in acute joint locking, and this is confirmed by the observation that all the joints afflicted by this condition are equipped with such structures.” pp. 90-91
In 1986, physical therapist Gregory Grieve authored a text titled Modern Manual Therapy of the Vertebral Column (8). This text boasts 61 international multidisciplinary contributors, contains 85 topic chapters, and is 898 pages in length. In the chapter titled “Acute Locking of the Cervical Spine” the text notes that a cause of acute cervical joint locking includes:
“Postulated mechanical derangements of the apophyseal joint include nipped or trapped synovial fringes, villi or meniscoids.” p. 351
In 1988, Rene Cailliet, MD, published the fourth edition of his book Low Back Pain Syndrome (9). At the time, Dr. Cailliet was the retired Chairman of the Department of Physical Medicine and Rehabilitation of the medical school at the University of California Los Angeles. Dr. Cailliet states:
“A meniscus exists within facet joints that becomes entrapped.”
as a cause of low back pain. He also includes an explanation of the benefits of spinal manipulation to treat the meniscal entrapment.
In the second edition of his blockbuster reference text, Common Vertebral Joint Problems, physical therapist Gregory Grieve includes a section on the meniscoid block. Mr. Grieve’s 1988 text is 787 pages in length and includes 2,472 references. Mr. Grieve (d. 2001) had been an Honorary Fellow of the Chartered Society of Physiotherapy and Clinical Tutor at the Department of Rheumatology and Rehabilitation at the Royal National Orthopaedic Hospital, London. While discussing Sudden Backache or Acute Lumbago, Greive’s text states (10):
“The small ‘meniscoid’ structures in the facet-joints are apparently susceptible to temporary impaction at times, with the chronic sequelae of the joint tissue damage probably adding to the natural process of senescence.” p. 201
“Impacted Synovial Meniscoid Villus”
“The patient with sudden backache due to presumed locking of a facet-joint is usually a young female but may be a young man, and there is often a degree of hypermobility. They often excel at athletics or ballet dancing, and during some activity which may be reaching up to open a window or adjust curtains, a lumbar synovial joint locks. No outside force is applied, the condition being consequent upon a body movement involving reaching or stretching. It is reasonable to suppose that the opposed joint faces of the hypermobile segment come apart more easily than usual, and the normally slight negative pressure within the joint cavity is further lowered by the greater distraction. A villus of synovial tissue is presumably ‘sucked in and nipped,’ and thus the meniscoid structure is impacted between joint surfaces. On resumption of normal posture the pain of impaction induces reactive muscle spasm, fixing the articulation rigidly to produce a locked joint.” p. 407
In her 1994 text Physical Therapy of the Cervical and Thoracic Spine, professor of physiotherapy from the University of South Australia, Ruth Grant writes (11):
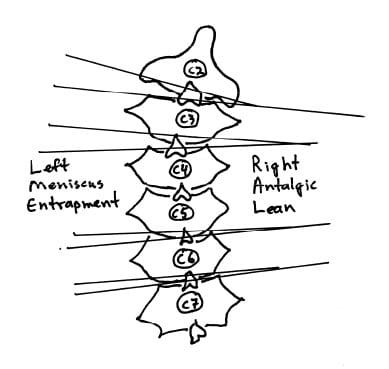
“Acute locking can occur at any intervertebral level, but is most frequent at C2-C3. Classically, locking follows an unguarded movement of the neck, with instant pain over the articular pillar and an antalgic posture of lateral flexion to the opposite side and slight flexion, which the patient is unable to correct. Locking is more frequent in children and young adults. In many, the joint pain settles within 24 hours without requiring treatment (because the joint was merely sprained or because it unlocked spontaneously), but other patients will require a localized manipulation to unlock the joint.” p. 298
In his 2004 text titled The Illustrated Guide to Functional Anatomy of the Musculoskeletal System (12), renowned physician and author Rene Cailliet, MD also comments on the anatomy of the interarticular meniscus. Dr. Cailliet is Professor emeritus at the University of Southern California School of Medicine and a clinical professor at the department of Physical Medicine Rehabilitation at the University of California Los Angeles (UCLA) School of Medicine. Dr. Cailliet writes:
“The uneven surfaces between the zygapophyseal processes are filled by an infolding of the joint capsule, which is filled with connective tissue and fat called meniscoids. These meniscoids are highly vascular and well innervated.” p. 95
In this comment, Dr. Cailliet, along with comments from Dr. James Fisk (3) and physical therapist Gregory Grieve (7) above, adds a critical feature to the understanding of the meniscoid block syndrome: the meniscus is “well innervated.” Presumably it is this innervation that produces the pain associated with meniscoid entrapments.
Physician, anatomist, and researcher Nikolai Bogduk from Australia has had a most distinguished career. A recent (September 2008) search of the National Library of Medicine database using the PubMed search engine found that Dr. Bogduk has written or contributed to 183 peer reviewed articles in the database. Additionally, Dr. Bogduk has written and contributed to dozens of reference texts pertaining to a variety of anatomic, orthopaedic, neurological, and clinical syndromes. In the fourth edition of his textbook Clinical Anatomy of the Lumbar Spine and Sacrum (13), Dr. Bogduk writes:
“The largest of the meniscoid structures are the fibro-adipose meniscoids. These project from the inner surface of the superior and inferior capsules. They consist of a leaf-like fold of synovium which encloses fat, collagen and some blood vessels.”
“Fibro-adipose meniscoids are long and project up to 5 mm into the joint cavity.” p. 35
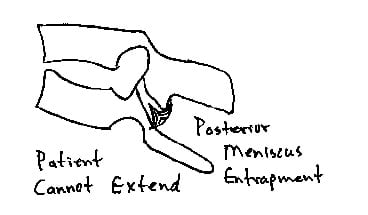
“A relatively common clinical syndrome is ‘acute locked back.’ In this condition, the patient, having bent forward, is unable to straighten because of severe focal pain on attempted extension.”
“Normal lumbar zygapophysial joints are endowed with fibroadipose meniscoids, and following trauma, segments of articular cartilage still attached to joint capsules may be avulsed from the articular surface to form an acquired cartilaginous meniscoid. These meniscoid structures could feasibly act as loose bodies within the joint or be trapped in the subscapsular pockets of the joints”
“Maintaining flexion is comfortable for the patient because that movement disengages the meniscoid. Treatment by manipulation becomes logical.”
“This condition of meniscoid entrapment is only theoretical, for it is difficult, if not impossible, to visualize meniscoids radiologically. However, it reigns as one of the plausible explanations for some cases of acute locked back, particularly those amenable to manipulative therapy.” p. 195
The January 15, 2007 publication of the top ranked orthopaedic journal Spine contains an article titled (14):
High-Field Magnetic Resonance Imaging of Meniscoids in the Zygapophyseal Joints of the Human Cervical Spine
Key Points From this article include:
1) Pain originating from the cervical spine is a frequent condition.
2) Neck pain can be caused by pathologic conditions of meniscoids within the zygapophysial joints.
3) “Cervical zygapophysial joints are well documented as a possible source of neck pain, and it has been hypothesized that pathologic conditions related to so called meniscoids within the zygapophysial joints may lead to pain.”
4) The meniscoids of the cervical facet joints contain nociceptors and may be a source of cervical facet joint pain.
5) Proton density weighted MRI image sequence is best for the evaluation of the meniscoid anatomy and pathology.
6) Meniscoids are best visualized with high-field MRI of 3.0 T strength.
7) Meniscoids are best depicted in a sagittal slice orientation.
8) The meniscoids in C1-C2 differ from those in the rest of the cervical spine.
9) Meniscoids may become entrapped between the articular cartilages of the facet joints. This causes pain, spasm, reduced movement, and “an acute locked neck syndrome.” “Spinal adjusting can solve the problem by separating the apposed articular cartilages and releasing the trapped apex.”
Although Dr. Bogduk (13) claims that these meniscoid blocks are “theoretical” because they cannot be visualized radiographically, recall that they have been demonstrated in anatomical sections, as shown in the text by Dr. Junghanns in 1971 (1). More recently, these articular meniscoids have been histologically documented and published in the 1988 text, Managing Low Back Pain by orthopaedic surgeon William H. Kirkaldy-Willis (d. 2006) (15). Dr. Kirkaldy-Willis was an emeritus professor from the Department of Orthopaedic Surgery, University Hospital, University of Saskatchewan College of Medicine. The 2007 article by physicians Freidrich (14) and colleagues in Spine further support that meniscoid entrapments are not “theoretical” because they can be imaged with proton density weighted MRI technology.
Clinical Applications
Decades of evidence support the perspective that the inner aspect of the facet capsules have a process that extends into and between the facet articular surfaces. This evidence includes anatomical sections, histological sections, MR imaging, and clinical evaluations. This meniscoid can become entrapped between the facet articulating surfaces, producing pain, spasm, and antalgia. Published terminology for the anatomy includes synovial fold, synovial villus, meniscoid, meniscoid block, and joint locking.
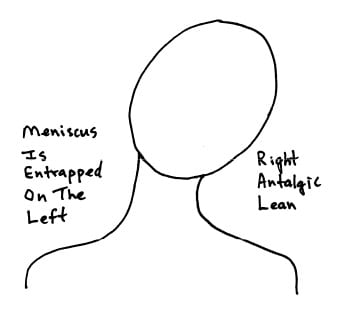
Using the cervical spine as a representative model, a classic clinical presentation would be that of an acute torticollis. If the meniscoid is entrapped on the left side of the cervical spine, the patient would present with an antalgia of right lateral flexion; in other words, the patient bends away from the side of entrapment. The patient’s primary pain symptoms will be on the side of entrapment, in this example, the left side. Active range of motion examination will show that the patient is capable of additional lateral flexion to the right, but will not laterally flex to the left because of increased pain; once again this is because the meniscus is entrapped on the left side and left lateral flexion increases meniscus compression, pain, and spasm. This is also why the patient is antalgic to the right; such positioning reduces left sided meniscus compression, pain, and spasm.
Additional clinical evaluation will reveal no sings of radiculopathy; no alterations of superficial sensation in a dermatomal pattern, and no signs of motor weakness or altered deep tendon reflexes. An important clinical feature is in that although the patient will not laterally flex the cervical spine to the left because of increased pain and spasm, left cervical lateral flexion against resistance without motion (the doctor holds the patient’s head so that there is no motion even though the left-sided cervical muscles are contracting) will not increase the patient’s pain. This is because the involvement is not muscular. Muscle contraction against resistance will not increase pain as long as the joint does not move in the meniscoid block syndrome.
A typical treatment protocol to manage the meniscoid block syndrome is that the patient is manipulated in an effort to free the entrapped meniscus. Post-graduate teachings in chiropractic orthopedics (Richard Stonebrink, DC, DABCO) and clinical experience indicate that the most successful manipulation would induce additional right lateral flexion; in other words, the manipulation would cause further right side antalgia. Such a maneuver would cause both a gapping of the facets on the left side as well as a tensioning of the left side facet capsules, together pulling free the entrapped meniscus. When the precise level of meniscoid entrapment is ascertained and that precise level is manipulated in the appropriate direction to cause the intended neurobiomechanical changes, it is referred to by chiropractors as a “spinal adjustment.” The depth and speed of such an adjustment must be sufficient to overcome local muscle spasm that reflexly exist as a consequence of the pain the patient is experiencing. Following this first manipulation/adjustment, the patient may benefit from 10-15 minutes of axial traction to the cervical spine. Experience suggests that most patients will benefit from the application of a soft cervical collar, worn continuously until the following day. The patient is evaluated and manipulated/adjusted again the second day, followed once again by optional axial cervical traction, but there is no need for the soft cervical collar on the second day. The patient is given the third day off, returning the fourth day for a final evaluation and adjustment/manipulation. It is typical for complete symptomatic resolution in a period of 3 – 5 days following onset and treatment.
An important caution in adjusting/manipulating the meniscoid block lesion is to not do so in such a manner that it straightens the right antalgic lean. Recall that the patient is antalgic to the right because the meniscoid is entrapped on the left side. To attempt to straighten the right antalgic lean out will increase the meniscoid compression, pain and spasm, making the patient truly unhappy. In contrast, the adjustment/manipulation should be made in such a manner that the right antalgic lean is enhanced, gapping the left sided articulations, freeing the entrapped meniscus, reducing pain and spasm.
As described in the eight edition of his book (1982) Textbook of Orthopaedic Medicine (16), orthopaedic surgeon Sir James Cyriax describes how the fibers of the multifidus muscles blend with the facet joint capsular fibers. Chiropractic orthopedic training indicates that at the beginning of any joint movement, appropriate local articular proprioception will quickly initiate a contraction of the multifidus muscle, tightening the capsular ligaments, and pulling the meniscus of that joint into such a position that it cannot become entrapped. This suggests that the etiology of the meniscoid block syndrome is a failure of appropriate proprioceptive driven reflexes, indicative of a long-standing biomechanical problem. It is reasonable and appropriate to treat the long-standing biomechanical problem with a more prolonged series of spinal adjustments/manipulations and indicated rehabilitation. Failure to do so often results in frequent reoccurrences of the meniscoid block syndrome following trivial mechanical environmental stresses.
References
1) Junghanns H; Schmorl’s and Junghanns’ The Human Spine in Health and Disease; Grune & Stratton; 1971.
2) Buerger AA and Tobis JS; Approaches to the Validation of Manipulation Therapy; Thomas, 1977.
3) Fisk JW; “An Evaluation of Manipulation in the Treatment of the Acute Low Back Pain Syndrome in General Practice” in Approaches to the Validation of Manipulation Therapy; Thomas, 1977.
4) Korr IM; Neurobiologic Mechanisms in Manipulative Therapy; Plenum; 1978.
5) Lewit K; “The Contribution of Clinical Observation to Neurobiological Mechanisms in Manipulative Therapy” in Korr IM; Neurobiologic Mechanisms in Manipulative Therapy; Plenum; 1978.
6) Lewit K; Manipulative Therapy in Rehabilitation of the Locomotor System, Butterworths, 1985.
7) Idczak GD; Aspects of Manipulative Therapy; Churchill Livingstone; 1985.
8) Grieve G; Modern Manual Therapy of the Vertebral Column; Churchill Livingstone; 1986.
9) Cailliet R; Low Back Pain Syndrome; FA Davis, 1988.
10) Grieve G; Common Vertebral Joint Problems, second edition; Churchill Livingstone; 1988.
(11) Grant R; Physical Therapy of the Cervical and Thoracic Spine, second edition; Churchill Livingstone, 1994.
(12) Cailliet R; The Illustrated Guide to Functional Anatomy of the Musculoskeletal System, American Medical Association, 2004.
(13) Bogduk N; Clinical Anatomy of the Lumbar Spine and Sacrum, fourth edition; Elsevier, 2005.
(14) Friedrich KM. MD, Trattnig S, Millington SA, Friedrich M, Groschmidt K, Pretterklieber ML; High-Field Magnetic Resonance Imaging of Meniscoids in the Zygapophyseal Joints of the Human Cervical Spine; Spine; January 15, 2007, Volume 32(2), January 15, 2007, pp. 244-248.
(15) Kirkaldy-Willis WH; Managing Low Back Pain, second edition; Churchill Livingstone, 1988.
(16) Cyriax J; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions, eighth edition; Bailliere Tindall, 1982.
