In 1935, Swedish physiologist Ulf von Euler isolated a biologically active compound from seminal fluid. He named the compound “prostaglandin” because he believed it was derived from the prostate gland. It is now known that prostaglandins are made in tissues throughout the body. [As an interesting side-note, von Euler (and colleagues) was awarded the Nobel Prize in Medicine or Physiology in 1970 for work on neurotransmitters.]
In 1971, biochemists Sune K. Bergström (Sweden; d.2004), Bengt I. Samuelsson (Sweden) and John R. Vane (United Kingdom; d. 2004) determined that aspirin-like drugs could inhibit the synthesis of prostaglandins. They subsequently jointly received the 1982 Nobel Prize in Physiology or Medicine for their research on prostaglandins. Their award was given:
“for their discoveries concerning prostaglandins and related biologically active substances”
The official the Nobel Prize press release made the following comments:
“Prostaglandins and related substances constitute part of a new biological system. They are formed from unsaturated fatty acids, primarily arachidonic acid. Arachidonic acid is present in the cellular membrane, which also has the enzymatic capacity to form prostaglandins. A release of these compounds takes place when the function of the tissue is perturbed by trauma, disease or stress.”
The prostaglandins and their related substances, which include thromboxane and prostacyclin, can therefore best be characterized as local tissue hormones.
“The latest members of the prostaglandin family [compounds made from arachidonic acid], the leukotrienes, are formed only in a few tissues and cells, chiefly in the lung and white blood cells. Release of leukotrienes in allergic and inflammatory conditions is probably responsible for the symptoms which characterize these diseases.”
Compounds inhibiting the formation of prostaglandins effectively relieve pains provoked by a number of conditions.
“Antiinflammatory compounds such as aspirin act by blocking the formation of prostaglandins and thromboxanes.”
“Prostaglandins are formed by conversion of unsaturated fatty acids, primarily arachidonic acid. The presence of these fatty acids in most cells in the body provided the basis for a new biological system of fundamental importance for several processes in the healthy and diseased body.”
“Aspirin and allied anti-inflammatory drugs block the synthesis of the prostaglandins.”
“Thanks to this important discovery the mode of action of aspirin, the most frequently used drug all over the world, was clarified.”
“Prostaglandins are continuously formed in the stomach, where they prevent the tissue from being damaged by the hydrochloric acid. If the formation of prostaglandins is blocked a peptic ulcer can rapidly be formed.”
If the release of prostaglandin E in the kidney is blocked, renal function rapidly deteriorates.
“The leukotrienes are formed in only a few tissues and cells, i.e. in the lungs and white blood cells, where they evidently play an important role for the development of allergic and inflammatory manifestations. It has recently been shown that leukotrienes are formed and released in lung tissue obtained from asthmatic patients and exposed to allergy provoking agents. They induce contraction of the bronchi and cause an accumulation of liquid in the lung, thus eliciting changes which are characteristic of the asthmatic attack. No doubt the discovery of the leukotrienes constitutes a breakthrough in the research on asthma. Compounds which block the formation of leukotrienes are also supposed to become effective anti-asthmatic drugs.”
“The cause of the often very severe pain during the menstruation periods has so far been unknown. However, it now seems as if this pain is due to an over production of prostaglandins in the uterus. Various compounds blocking the synthesis of prostaglandins have therefore been used and found to effectively reduce this pain. Similarly, these compounds are also superior in reducing pains induced by stones in the gallbladder and kidney. Thus, a completely new type of treatment against severe pain has been established.”
As a consequence of the 1982 Nobel Prize in Medicine or Physiology, scientists and healthcare providers have a much better understanding of the mechanisms of how aspirin and other nonsteroidal antiinflammatory drugs reduce pain. However, the same Nobel Prize winning physiology notes that these same products that reduce pain may increase the risk for gastrointestinal bleeding and kidney damage. More recently, these products have been linked to increased cardiovascular risks, and even to an increased risk in Alzheimer’s dementia. A few selected reviews follow:
Kidney Disease
Risk of Kidney Failure Associated with the Use of Acetaminophen, Aspirin, and Nonsteroidal Antiinflammatory Drugs
New England Journal of Medicine
December 22, 1994
Number 25, Volume 331:1675-1679
Thomas V. Perneger, Paul K. Whelton, and Michael J. Klag
These authors note “people who take analgesic drugs frequently may be at increased risk of end-stage renal disease (ESRD), but the extent of this risk remains unclear.” Therefore, they studied 716 patients treated for ESRD and 361 control subjects of similar age. The results showed that a cumulative dose of 5,000 or more pills containing NSAIDs was associated with an increased risk of ESRD by 780% compared to the control population. Because the risk was associated only with those taking large doses of NSAIDs (5,000 or more cumulative dose), the risk is associated with chronic conditions. This finding “arouses concern about the safety of persons taking large quantities of NSAIDs.”
Gastrointestinal Bleeding
Gastrointestinal Toxicity of Nonsteroidal Antiinflammatory Drugs
The New England Journal of Medicine
June 17, 1999
Michael Wolfe, M.D., David R. Lichtenstein, M.D., Gurkirpal Singh, M.D.
These authors are from the Section of Gastroenterology, Boston University School of Medicine and Boston Medical Center Division of Immunology and Rheumatology, and Stanford University School of Medicine. The article has 113 references. The authors make the following points:
Aspirin was the first nonsteroidal anti-inflammatory drug (NSAID) to be synthesized, one hundred years ago, by the Bayer Industries. Forty years later there was endoscopic proof that aspirin could cause gastric mucosal damage, which has been substantiated by numerous other reports. The introduction of more potent NSAID agents increases the propensity for toxic effects. NSAID agents constitute one of the world’s most widely used classes of drugs, with more than 70 million prescriptions and more than 30 billion over-the-counter tablets sold annually in the United States.
“It has been estimated conservatively that 16,500 NSAID-related deaths occur among patients with rheumatoid arthritis or osteoarthritis every year in the United States.” “If deaths from gastrointestinal toxic effects of NSAIDs were tabulated separately in the National Vital Statistics reports, these effects would constitute the 15th most common cause of death in the United States. Yet these toxic effects remain largely a ‘silent epidemic,’ with many physicians and most patients unaware of the magnitude of the problem. Furthermore, the mortality statistics do not include deaths ascribed to the use of over-the-counter NSAIDs.”
Doses of aspirin as low as 30 mg are sufficient to suppress prostaglandin synthesis in the gastric mucosa initiating gastric-duodenal mucosal injury, resulting in the release of oxygen-derived free radicals. “In the majority of patients, NSAID-induced gastroduodenal mucosal injury is superficial and self-limited. However, peptic ulcers develop in some patients, and they may lead to gastroduodenal hemorrhage, perforation, and death.”
Epidemiology of NSAID induced gastrointestinal complications
Journal of Rheumatology
April 1999
26 Suppl 56:pp. 18-24
Gurkirpal Singh, George Triadafilopoulos
These authors are from the Department of Medicine, Division of Immunology, Stanford University School of Medicine. These authors note:
“Nonsteroidal anti-inflammatory drugs (NSAID) are one of the most commonly used classes of medications worldwide. It is estimated that more than 30 million people take NSAID’s daily. Gastrointestinal (GI) complications related to NSAID therapy are the most prevalent category of adverse drug reactions. Patients with arthritis are among the most frequent users of NSAID’s and are therefore particularly at risk for these side effects.”
In this prospective observational study, which involved more than 36,000 patients with rheumatic diseases from 17 centers in the United States and Canada who have been followed for more than 300,000 patient-years, they found that “serious GI complications can occur without any prior side effects or prior evidence of mucosal damage.” Conservatively, the number of hospitalizations for serious GI complications per year is estimated to be 103,000, with a conservative estimated cost of $15,000 to $20,000 per hospitalization, the annual costs exceed $2 billion. “The overall estimates for NSAID-related deaths among patients with RA and OA are even more startling. It is conservatively estimated that 16,500 NSAID-related deaths occur in these patients every year in the United States.”
Cardiovascular Events
Most of us recall the voluntary withdrawal of the Cox-2 inhibitor Vioxx on September 30, 2004 as a consequence of evidence of the unacceptable risk of cardiovascular events. Consequently, other COX inhibition drugs were evaluated for cardiovascular safety. One such study is presented here:
NSAID use and the risk of hospitalization for first myocardial infarction in the general population: a nationwide case-control study from Finland
European Heart Journal
July 2006;27(14):1657-63
Helin-Salmivaara A, Virtanen A, Vesalainen R, Grönroos JM, Klaukka T, Idänpään-Heikkilä JE, Huupponen R.
These authors are from the Centre for Pharmacotherapy Development and Postgraduate School of Clinical Drug Research, University of Turku, Helsinki, Finland. The abstract from their article includes the following:
AIMS: To evaluate the risk of first myocardial infarction (MI) associated with the use of various non-steroidal anti-inflammatory drugs (NSAIDs) in the general population.
METHODS AND RESULTS: We conducted a population-based matched case-control study over the years 2000-3 in outpatient residents of Finland and compared them to 138,949 controls.
For combined NSAIDs, the adjusted odds ratio for the risk of first MI with current use was 1.40 (40% increased risk).
Age of current user did not consistently modify the risk.
No NSAID was associated with an MI-protective effect.
All durations from 1 to 180 days of conventional NSAIDs and from 31 to 90 days duration of COX-2 selective NSAIDs were associated with an elevated risk of MI.
CONCLUSION: Current use of all NSAIDs is associated with a modest risk of first time MI.
Dementia, including Alzheimer’s disease
Risk of dementia and AD with prior exposure to NSAIDs in an elderly community-based cohort
Neurology
[April 22, 2009, early publication]
J.C.S. Breitner, MD, MPH, S.J.P.A. Haneuse, PhD, R. Walker, MS, S. Dublin, MD, PhD, P.K. Crane, MD, MPH, S.L. Gray, PharmD, M, E.B. Larson, MD, MPH. These authors are associated with the University of Washington School of Medicine.
These authors studied 2,736 dementia-free elderly enrollees for up to 12 years to identify dementia and Alzheimer’s disease (AD). “Contrary to the hypothesis that NSAIDs protect against AD, pharmacy-defined heavy NSAID users showed increased incidence of dementia and AD, by 66%. These numbers represent only the use of prescription NSAIDs; over-the-counter use was more difficult to track and was assessed only indirectly. Sixteen different prescription NSAIDs were consumed, and 46% was one drug, Ibuprofen; a standard daily dose of prescription ibuprofen was defined as 1,200 mg per day. This is obtained by consuming two 600 mg prescription capsules per day.
2,736 subjects use (1,200 mg per day) of prescription NSAIDs (rounded)
| Beginning of Study | 12 Years Later | |
|
Light Use |
50% | 41% |
|
Moderate Use |
37% | 42% |
|
Heavy Use |
13% | 17% |
This indicates that as time progressed, subjects increased their use of NSAIDs.
“Alzheimer disease (AD) is a large and growing public health problem and disease prevention represents the best long-term strategy for reducing its human and economic toll.” “Presently no curative therapies exist, but even a small delay in disease onset would have significant public health implications.” This study is important because it included “nearly 17,000 person-years of follow-up.” This study showed that over 50% of senior citizens are consuming moderate to heavy doses of NSAIDs, and that there are very few elderly Americans who do not consume NSAIDs.
In this very well done study, elderly persons who were heavy users of NSAIDs were 66% more likely to have dementia and 57% more likely to have Alzheimer’s disease compared to nonusers of the drugs. “In a large cohort study of an elderly population-based sample, we observed no reduction in risk of dementia or AD among users of NSAIDs. Instead, we found that prior sustained NSAID exposure was associated with increased incidence of dementia and AD. This result was robust to comprehensive sensitivity analyses investigating features of both the design and analytic approach.”
Despite these health risks associated with long-term use of NSAIDs, a recent analysis of NSAID use in the United States was published in the May 3, 2008 issue of the journal The Lancet. The article is authored by AB Krueger and AA Stone from the Economics Department of Princeton University, and is titled:
Assessment of Pain: A community-based diary in the United States
This analysis indicates that at any given point in time, as many as 28% of Americans are suffering from pain, and their primary management of that pain is by the consumption of NSAIDs. The article estimates that NSAID consumption by these individuals approaches $15 billion per year in prescription NSAIDs and an additional $2 billion per year in over-the-counter NSAIDs. One wonders if there are any management options that are at least as effective as NSAIDs with fewer adverse health risks.
Simplified Review Of Biochemistry
Both omega-6 and omega-3 fatty acids are essential for human health, and our bodies do not have the ability to create them from other fatty acids. Consequently, both omega-6 and omega-3 fatty acids must be consumed in the diet. Dietary deficiencies in either omega-6 or omega-3 fatty acids are deleterious to our health.
Additionally, the ratio of omega-6 to omega-3 fatty acids is critically important. “Historical estimates place the ratio of omega-6 to omega-3 oils at nearly 1:1 for prehistoric humans.” The ratio of omega-6 to omega-3 fatty acids has changed dramatically due to the widespread use of vegetable oils (mostly n-6 fats) in cooking and foods. By 1900, the ratio of omega-6 to omega-3 fatty acids had increased to about 4:1. The current American ratio is about 25:1. This “sharp rise is due to increased vegetable oil consumption: from 2 lb. per year in 1909 to 25 lb. per year in 1985!” (Mark Boswell and B. Eliot Cole, editors; American Academy of Pain Management Weiner’s Pain Management, A Practical Guide for Clinicians; Seventh Edition, 2006, pp.584-585.)
An important aspect of essential fatty acid biology is that the 20-carbon long omega-6 and omega-3 fatty acids are the precursors to a group of powerful but short-lived hormone-like compounds called “eicosanoids.” One category of eicosanoids is referred to as “prostaglandins.” Another group is referred to as “leukotrienes.” Clinical applications of this biochemistry is summarized in the following pictures:
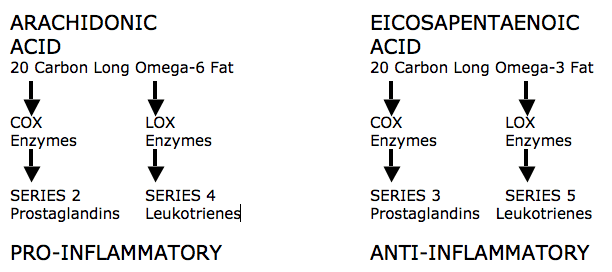
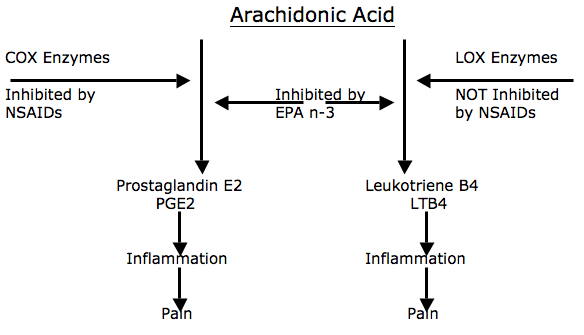
Historically, the conversion of arachidonic acid into pro-inflammatory prostaglandin E2 has been inhibited by utilization of nonsteroidal anti-inflammatory drugs (NSAIDs) that block the cyclo-oxygenase (COX) enzymes. However, as noted in the article reviews above, long-term use of these drugs can cause problems in some patients. Additionally, the article reviews below indicate that nonsteroidal anti-inflammatory drugs (NSAIDs) do not inhibit the lipo-oxygenase (LOX) pathway and therefore do not inhibit the formation of pro-inflammatory series 4 leukotrienes. In contrast the omega-3 fatty acid Eicosapentaenoic acid (EPA) inhibits both cyclo-oxygenase (COX) and lipo-oxygenase (LOX) enzymes, reducing the production of both pro-inflammatory prostaglandin E2 and series 4 leukotrienes.
Alternative Approach #1
Fish Oil
Fish contains omega-3 polyunsaturated fatty acids, including the 20-carbon long oil eicosapentaenoic acid, or EPA. As noted above, EPA has a therapeutic advantage over NSAIDs in that it inhibits both the COX and LOX enzymes, reducing the production of both PGE2 and LTB4 proinflammatory eicosanoids. Additionally, EPA is also the precursor to the antiinflammatory eicosanoid prostaglandin E3, or PGE3.
In 2006, Pittsburgh neurosurgeon and specialist in spinal degenerative disease, Joseph Maroon, MD, published an appropriate study to this discussion, as follows:
Omega-3 Fatty acids (fish oil) as an anti-inflammatory:
an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain
Surgical Neurology
65 (April 2006) 326– 331
This paper won first prize in the poster competition at the American Association of Neurological Surgeons Annual Meeting, New Orleans, LA, April 2005. The authors, Joseph Maroon, MD, Jeffrey Bost, PAC, are from the Department of Neurological Surgery, University of Pittsburgh Medical Center. Dr. Maroon also wrote a book on the same topic in 2006, titled:
Fish Oil, The Natural Anti-Inflammatory
Joseph Maroon, MD, Basic Health, 2006
Additionally, Dr. Maroon is the neurosurgeon for the 2009 Super Bowl Champion Pittsburgh Steelers.
In this article, Dr. Maroon reviews how the use of NSAIDs is associated with occasional extreme complications, including gastric ulcers, bleeding, myocardial infarction, stroke, and even death. He states:
“NSAIDs are the most common cause of drug-related morbidity and mortality reported to the FDA and other regulatory agencies around the world.”
“More than 70 million NSAID prescriptions are written each year, and 30 billion over-the-counter NSAID tablets are sold annually.”
“The agent best documented by hundreds of references in the literature for its anti-inflammatory effects is omega-3 EFAs found in fish and in pharmaceutical-grade fish oil supplements.”
“To encourage the production of anti-inflammatory PGs and to discourage the production of inflammatory PGs, saturated fats, trans-fatty acids, and arachidonic acid should be reduced in the diet; blood glucose should be controlled; and appropriate amounts of omega-3 fatty acids found in fish oils should be consumed.”
“Omega-3 EFA fish oil supplements appear to be a safer alternative to NSAIDs for treatment of nonsurgical neck or back pain.”
In this study, Dr. Maroon showed that after 75 days on high dose fish oil, 59% of patients with chronic spinal pain and who had degenerative spine disease were able to discontinue their prescription NSAIDs, and 88% stated they were satisfied with their improvement and that they would continue to take the fish oil.
In 2006, Leslie G Cleland, Michael J James and Susanna M Proudman wrote:
Fish oil: what the prescriber needs to know
Arthritis Research & Therapy
Volume 8, Issue 1, 2006, pp. 402
In 2007, Robert J. Goldberg and Joel Katz wrote:
A meta-analysis of the analgesic effects of omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain
Pain
May 2007, 129(1-2), pp. 210-223
These two articles agree that in order to achieve an antiinflammatory effect from fish oil consumption, one must consume a minimum of 2.7 g per day of EPA + DHA, and daily consumption of this amount must be continued for a period of a minimum of 2 – 4 months. Both articles claim that consumption of less than 2.7 g per day of EPA + DHA and/or consumption for a period of less than 2 months would not be beneficial when striving for an antiinflammatory benefit.
Biochemist Barry Sears, PhD, has written three books on the omega-3 topic:
The Omega Zone, by Barry Sears, Regan Books, 2002
The Anti-Inflammation Zone, by Barry Sears, PhD, Regan Books, 2005.
Toxic Fat, Barry Sears, PhD, Regan Books, 2008.
Dr. Sears claims that if one is dealing with chronic pain, better clinical outcomes will occur if the patient consumes 5 g per day of EPA + DHA. He also claims that omega-3 dosing can be fine tuned by assessing the blood ratio of arachidonic acid/eicosapentaenoic acid (AA/EPA). In review, arachidonic acid is a 20-carbon long omega-6 fatty acid and eicosapentaenoic acid is its competing 20-carbon long omega-3 fatty acid. Dr. Sears gives the following guideline:
| Dangerous | Poor | Good | Ideal | |
| AA/EPA | >15 | 10 | 3 | 1.5 |
Dr. Sears refers to arachidonic acid as “toxic fat”. Because of the contemporary abundance of arachidonic acid or its omega-6 plant based precursors in our diets, Dr. Sears, Harvard psychiatrist Andrew Stoll, MD, PhD (Omega-3 Connection, Simon & Schuster, 2001), and geneticist Artemis P. Simopoulos, MD (Omega-3 Fatty Acids and Athletics; Current Sports Medicine Reports; July 2007, 6:230–236) all recommend that the best results will be achieved with fish oil consumption if there is higher levels of EPA. Specifically, they each recommend that the EPA/DHA ratio be at least 2/1.
Alternative Approach #2
Spinal Manipulation
In 1985, Dr. Kirkaldy-Willis, a Professor Emeritus of Orthopedics and director of the Low-Back Pain Clinic at the University Hospital, Saskatoon, Canada, co-authored:
Spinal Manipulation in the Treatment of Low back Pain
Canadian Family Physician
March 1985, Vol. 31, pp. 535-540
In this article, Dr. Kirkaldy-Willis suggests that the clinical benefit of spinal manipulation is linked to an improved range of motion. This improved range of motion subsequently “closes” the pain gate, as originally described by Ronald Melzack and Patrick Wall in 1965.
In 2003, Giles and Muller published:
Chronic Spinal Pain:
A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation
Spine July 15, 2003; 28(14):1490-1502
In this study the medications used were prescription NSAIDs Celebrex or Vioxx. The spinal manipulation used was delivered by chiropractors. All patients were assessed using standard measurement outcomes. The 9-week follow-up analysis is summarized below:
| Treatment | Drugs (Celebrex or Vioxx) | Acupuncture | Chiropractic Adjustments |
| Years Of Chronic Spinal Pain | 4.5 or 6.4 | 4.5 or 6.4 | 8.3 |
| % Asymptomatic within 9 weeks | 5% | 9.4% | 27.3% |
| % That suffered an adverse event | 6.1% | 0% | 0% |
The authors concluded:
The highest proportion of early (asymptomatic status) recovery was found for manipulation (27.3%), followed by acupuncture (9.4%) and medication (5%).
“The results of this efficacy study suggest that spinal manipulation, if not contraindicated, may be superior to needle acupuncture or medication for the successful treatment of patients with chronic spinal pain syndrome.”
“In summary, the significance of the study is that for chronic spinal pain syndromes, it appears that spinal manipulation provided the best overall short-term results, despite the fact that the spinal manipulation group had experienced the longest pretreatment duration of pain.”
In summary, it has been know for decades that long-term consumption of NSAIDs is associated with undesirable and potentially fatal side effects. It has also been shown that both fish oil supplementation and spinal manipulation can be beneficial to individuals suffering from chronic spinal pain syndromes. These alternative approaches to the management of chronic spinal pain syndromes may be appropriate and beneficial for some patients, resulting in good outcomes with very low risks.
