Dr. Ruth Jackson had such an accomplished life that shortly after her death in 1994 she was profiled in both the American Journal of Bone and Joint Surgery (1) in 1995 and in the Iowa Orthopedic Journal in 2001 (3).
Dr. Jackson’s profile in the Journal of Bone and Joint Surgery was simply titled:
RUTH JACKSON, M.D. 1902-1994
“Ruth Jackson, a prominent orthopaedic surgeon, died on August 28, 1994, in Dallas, Texas.”
Ruth Jackson was born in 1902, graduated from high school in 1920, and attended the University of Texas at Austin, where her major was sociology. In her junior year, while on a class assignment to see if a poor family needed groceries, she noted that the father could not work because of a knee problem. In her desire to help with such problems she switched to a premedical major, graduating in 1924 with a Bachelor’s degree in zoology and a minor in chemistry. She then entered Baylor University College of Medicine in Dallas as one of only four women in a class of 164.
“While in medical school, Ruth protested that women were not allowed to examine male patients and suggested that a woman planning to practice medicine required the same firsthand knowledge of men as a future male physician needed of women. She graduated in 1928, ranked eighth in her class.”
Dr. Jackson accepted a residency in orthopaedics at the University of Iowa, and began working with crippled children. She began her private practice in Dallas in 1932.
“When The American Academy of Orthopaedic Surgeons was founded in 1933, all practicing male orthopaedic surgeons were automatically admitted as members. However, Dr. Jackson was told that she could become a member only if she passed the Board examination. Undaunted, she completed this requirement in 1937 and thus became the first woman to be admitted to The Academy. She was also the first woman to be certified by the American Board of Orthopaedic Surgery.”
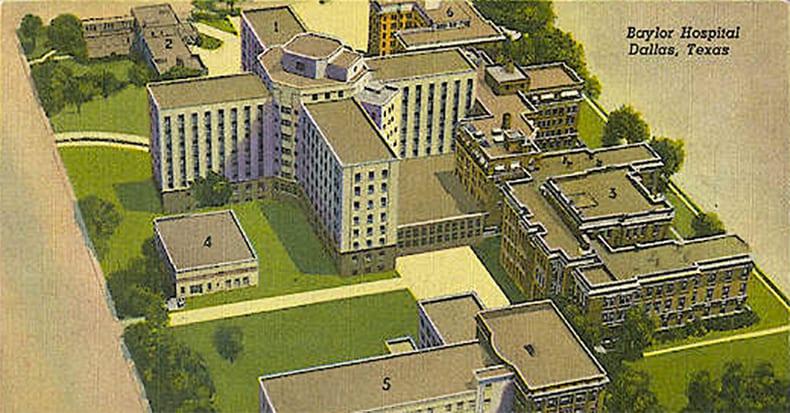
“From 1936 to 1941, Dr. Jackson was Chief of Orthopaedics at Parkland Hospital in Fairmont. In 1945, she had her own private clinic built in Dallas. The clinic comprised several examining rooms, an operating room, physical therapy facilities, and a radiology suite. She conducted her medical practice in these offices for the next thirty-eight years, performing all operations, including lumbar discectomy, with use of local anesthesia.”
Dr. Jackson had a special interest in injuries of the cervical spine. Her interest arose after a neck injury she sustained in a motor-vehicle accident. To treat these “whiplash” injuries, she invented the Jackson Cervi-Pillow. In 1956 she published her acclaimed, authoritative book entitled The Cervical Syndrome. The fourth and final edition of her book was published in 1978 (2).
In her career, Dr. Jackson published more than twenty-five articles, and she lectured extensively in the United States and throughout the world. Two of her articles pertaining to cervical spine trauma are reviewed below.
Dr. Jackson’s other noted professional accomplishments include:
- She started The Ruth Jackson Research Foundation at Baylor University.
- She funded the Ruth Jackson Visiting Professorship at Baylor University, starting in 1961.
- She established the Ruth Jackson Library at Baylor University.
- The Ruth Jackson Orthopaedic Society was founded in 1983. It currently has more than 500 members. This organization salutes her pioneering spirit and her accomplishments and seeks to advance the careers of women in orthopaedics.
Dr. Jackson retired from clinical practice in 1989 at the age of 87 years.
••••
Dr. Ruth Jackson’s profile in the Iowa Orthopedic Journal was titled (3):
RUTH JACKSON, M.D.:
A WOMAN OF DETERMINATION AND ACCOMPLISHMENT
Additional information from this profile indicates that her whiplash injury occurred in 1936. Subsequently:
“She had significant cervical pain for several years and that experience stimulated her interest in cervical spine problems.”
The article indicates that Dr. Jackson had treated over 15,000 patients with cervical spine problems.
••••
In her career, Dr. Jackson published six studies in the medical literature pertaining to cervical spine trauma, as follows:
1) The Cervical Syndrome As a Cause of Migraine. Journal of the American Medical Women’s Association. December 1947, Vol. 2, No. 12, pp. 529-534.
2) The cervical syndrome. Dallas Medical Journal. 1949 Oct;35(10):139-46.
3) The Positive Findings in Alleged Neck Injuries. American Journal of Orthopedics. 1964 Aug-Sep;6:178-87.
4) Headaches associated with disorders of the cervical spine. Headache. 1967 Jan;6(4):175-9.
5) Traumatic arthritis of the cervical spine. Comprehensive Therapy. 1981 Feb;7(2):58-61.
6) Cervical trauma: not just another pain in the neck. Geriatrics. 1982 Apr;37(4):123-6.
Two of these articles are reviewed below:
The Cervical Syndrome As a Cause of Migraine
Journal of the American Medical Women’s Association
December 1947, Vol. 2, No. 12, pp. 529-534
In this article, Dr. Jackson makes the following key points:
1) At least half of patients suffering from cervical syndrome causing shoulder disability will also complain of headache as one of their principle symptoms.
2) The cervical syndrome is caused by “cervical nerve root irritation.”
3) There is a relationship between the cervical syndrome, cervical nerve root irritation, and the sympathetic nervous system. It is this sympathetic nervous system involvement that is responsible for headaches, including migraine.
4) “The cervical nerve roots are more vulnerable to pressure or irritation from ruptured discs, hemorrhage, inflammatory processes of the capsules, spurs, and abnormal motion of the joints due to relaxation or tearing of the capsular and ligamentous structures.”
5) Sympathetic nerves that originate at the T1 and T2 levels ascend into the cervical spine becoming the cervical sympathetic trunk, with its inferior, middle, and superior ganglia. From the superior cervical sympathetic ganglia, post-ganglionic sympathetic efferents pass to the anterior rami of the upper four cervical nerves. Other postganglionic sympathetic fibers travel via the internal carotid and ophthalmic arteries to join the orbit and supply the dilator muscle of the pupil and smooth muscles of the upper eyelid, the back of the orbit, and the blood vessels of the eyeball. It is the irritation of these sympathetic nerves in the cervical spine that gives rise to migraine-type headaches.
6) “Irritation of the cervical nerve roots before they divide into anterior and posterior primary rami may occur as a result of any mechanical derangement in or about the intervertebral foramina. The most common cause of irritation is abnormal motion or subluxation of the joints due to relaxation of the capsular and ligamentous structures following trauma.”
7) Following whiplash trauma, as time passes, “abnormal motion or subluxations of the articular processes, will cause irritation of one or more nerve roots.”
8) “Any unguarded motion or prolonged relaxation of the neck in one position may allow a subluxation to occur,” which may cause cervical nerve root irritation.
9) Cervical trauma can cause chronic pain syndrome, including pain decades later.
10) Approximately 2/3 of the patients with neck symptoms are women.
11) As a consequence of increased mobility and reduced stability of the upper cervical spine, the C1-C2-C3 nerve roots are most vulnerable to irritation. When the C1-C2-C3 nerve roots are involved, typical symptoms include:
A)) Neck pain
B)) Limitation of neck motion
C)) Headache, which usually “starts at the back of the neck or base of the skull and then involves one or both sides of the head, and pain in the mastoid region or in the ears”
D)) Blurring of the vision (found in 20% of patients)
E)) Dizziness and nausea
F)) Numbness of the sides of the neck
G)) Tightness of the neck muscles
H)) Pain in the supraclavicular region
12) “If C4 is involved there may be shortness of breath, palpitations, anterior chest pain and pain and muscle spasm in the muscles supplied by C4.”
13) “When the lower nerve roots are involved, the symptoms are commensurate with the segmental character of the nerve roots which are irritated.” These patients often have numbness or tingling of the fingers when they awaken.
14) “There is always tenderness to deep pressure over the vertebrae, usually just lateral to the spinous process of the side of the nerve root irritation.” “If the irritation is above the fourth nerve root there may be tender areas over the occiput and the mastoid. If the fourth nerve root is involved, there may be tender areas in the ridge of the trapezius and/or in the sternomastoid muscles.” Irritation of the fourth nerve root may also cause referred pain to the diaphragm, the pericardium, and shoulder.
15) “The most constant finding in all of our cases was the presence of myalgic areas in the upper or lower cervical portion of the rhomboid muscles which is indicative of fifth nerve root irritation.”
16) “Often there seems to be localized fibrosis of the muscle. Irritation causes spasm which if allowed to persist causes ischemia with eventual formation of localized fibrosis.”
17) Dr. Jackson stresses the importance of cervical spine x-rays in cases of cervical spine trauma. She especially emphasizes the importance of maximum flexion and maximum extension lateral views. The abnormal forward or backward slipping of a vertebral segment on flexion or extension is called a “subluxation.”
18) 96% of patients with cervical syndrome headaches will show subluxations at more than one level, and in 77% the subluxation was of C2 on C3, irritating the C3 nerve root. “This indicates that the irritation of the third cervical nerve root must have been responsible for the greatest percentage of headache.” “Cervical nerve root irritation (C3 usually) is an etiological factor in migraine.”
19) Dr. Jackson believes that the blurring of the vision (and ipsilateral pupil dilation, when present) seen in many cervical syndrome/headache patients is caused by irritation of the superior sympathetic ganglion caused by cervical muscle spasm.
20) Irritation of the cervical nerve roots will cause spasm of the associated cervical spine muscles. Spasm of the muscles that surround the superior sympathetic ganglia causes irritation to both the ganglia and/or the postganglionic sympathetic fibers. This sympathetic irritation can in turn cause symptoms of migraine-like headache.
21) Injured patients should use a cervical contour pillow for rest and healing. “This pillow has been our greatest adjunct in the treatment of cervical nerve root irritation.”
SUMMARY AND CLINICAL SIGNIFICANCE
In this article, Dr. Jackson stresses that the physiological basis for neck-shoulder-headache complaints is cervical nerve root irritation. She stresses that the cervical nerve roots are quite vulnerable to pressure or irritation from ruptured discs, hemorrhage, inflammatory processes of the capsules, spurs, and abnormal motion of the joints due to relaxation or tearing of the capsular and ligamentous structures.
Irritation of the cervical nerve roots occurs as a result of any mechanical derangement in or about the intervertebral foramina. The most common cause of irritation is abnormal motion or subluxation of the joints due to relaxation of the capsular and ligamentous structures following trauma. Following whiplash trauma, as time passes there is an increased probability of abnormal motion or subluxations of the articular processes, which will cause irritation of one or more nerve roots. Additionally, any unguarded motion or prolonged postural distortion of the neck may allow a subluxation to occur, causing irritation of a cervical nerve root.
Irritation of the cervical nerve roots will cause spasm of the associated cervical spine muscles. Spasm of the muscles that surround the superior sympathetic ganglia causes irritation to both the ganglia and/or the postganglionic sympathetic fibers. This sympathetic irritation can in turn cause symptoms of migraine-like headache.
Additionally, this nerve root irritation and attendant muscle spasm, if not properly treated, causes muscle ischemia with eventual formation of localized fibrosis. This muscle spasm can prolong symptoms and lead to chronicity of symptoms.
Diagnostically, Dr. Jackson insists on acquiring cervical spine stress (maximum flexion-extension) radiographs. She notes that such x-rays can display abnormal forward or backwards slippage of the vertebral segments. Such abnormal movement is once again associated with increased nerve root irritation and symptoms.
A physical diagnostic indicator of cervical nerve root irritation is tenderness to deep pressure over the vertebrae, usually just lateral to the spinous process of the side of the nerve root irritation.
Fortunately, post-traumatic cervical nerve root irritation and its associated abnormal segmental mobility (subluxations), muscle spasm, and even chronic muscle fibrosis are treatable. Chiropractic approaches to such problems include passive manual mobilizations, exercise, soft tissue work, myotherapy, traction, and joint manipulation (adjustments).
••••
The Positive Findings In Neck Injuries
American Journal of Orthopedics
August-September, 1964, pp. 178-187
In this article, Dr. Jackson makes the following key points:
1) 90% of neck disorders are caused by trauma.
2) Of the trauma cases, 85% are caused by motor vehicle collisions.
3) “The forces which are imposed on the cervical spines of the passengers of colliding vehicles are tremendous, and if one attempts to calculate mathematically the amount of such forces, the results are unbelievable.”
4) Dr. Jackson emphasizes the lack of relationship between vehicle damage and passenger injury. She states:
“The damage to the vehicles involved in collisions is no indication of the extent of the injuries imposed on the passengers.”
“The extent of damage to the vehicles is in no way proportional to the extent of damage imposed upon the cervical spines of the passengers.”
5) “Healing of sprained ligamentous structures takes place by the formation of scar tissue which is less elastic and less functional than normal ligamentous tissue.” Therefore, sprains result in some degree of permanent injury.
6) “Injuries of the intervertebral disc structures are frequent and they may vary from a slight rent in the annulus fibrosis to a complete avulsion of the disc from its attachments.”
7) “Any injury of the disc causes a disturbance in the dynamics of the motor unit of which the disc is a part. This leads to degeneration of the disc and the proximate joints.”
8) The nerve roots, the cervical sympathetic nerves and the spinal cord may suffer injuries of varying degrees.
9) The location of segmental motion problems can be verified by lateral radiographs of the cervical spine in maximum flexion and extension.
10) Upper extremity deep tendon reflexes may be hyperactive immediately following neck injury, but after a few days they may become hypoactive.
11) Superficial sensation may initially be hyperesthesia, but after a few weeks may become hypoesthetic.
12) Grip strength should be measured by a dynamometer, and should be performed 4 times in sequence to look for muscle fatigue. Normally each of the 4 readings should be essentially the same.
13) Unilateral dilation of the pupil “indicates irritation of the sympathetic nerve.”
14) Whiplash-caused partial deafness may be improved with cervical traction.
15) “Irritation of the cervical sympathetic nerve supply may give rise to vasoconstriction of the arteries which are supplied by the sympathetic fibers.” Blood pressure in the two arms often varies as much as 10 – 20 points following neck injuries. This is a completely objective finding.
16) Pre-existing pathological conditions of the cervical spine, when injured, “result in more damage than would be anticipated in a so-called ‘normal’ cervical spine.”
17) Dr. Jackson notes that in order to ascertain injuries, an “adequate radiographic examination is essential.” She recommends 8 x-rays be exposed following whiplash trauma, including an AP cervical with a “caudad-angled view.” This view “may show fractures of the laminae and of the inter-articular isthmuses which may not be demonstrable in any other view.” She also notes that initial x-rays may be normal, but subsequent x-rays may reveal multiple problems; therefore, repeat x-rays are essential. Dr. Jackson states:
“All radiographs should be repeated periodically. Subsequent findings may be very revealing.”
18) X-rays showing “any segmental instability, any segmental restriction of motion, and any segmental angulation may indicate severe injury.”
19) The intervertebral foramina may suffer from encroachment as the result of “hemorrhage, swelling, or hyperplasia of the proximate capsular and ligamentous structures,” even in the presence of normal oblique x-rays.
21) The alar ligaments of the upper cervical spine are very vulnerable to injury.
22) “Repeated physical and radiographic examinations are necessary for final analysis.”
SUMMARY AND CLINICAL SIGNIFICANCE
Dr. Ruth Jackson was one of the most experienced clinicians in world history pertaining to whiplash trauma to the cervical spine. In this article she repeatedly states the observation that there is no relationship between vehicle damage and passenger injury. She also makes the important observation that pre-existing pathological conditions of the cervical spine, when injured, “result in more damage than would be anticipated in a so-called ‘normal’ cervical spine.” Although these observations were made nearly half a century ago, these concepts remain contentious today and a point of frustration for both patients and clinicians who are thrust into the med-legal arena when caring for whiplash-injured patients.
Once again, Dr. Jackson emphasized the relationship between cervical spine trauma and irritation of the cervical nerve roots. Cervical spine nerve root irritation often affects the function of the sympathetic nervous system, either directly or indirectly as a consequence of muscle spasm. Sympathetic nerve irritation is in turn associated with cranial symptoms, including headaches.
Sadly, Dr. Jackson observes that injured soft tissues often display healing problems, helping to explain why some whiplash-injured patients suffer from long-term symptoms. She states:
“Healing of sprained ligamentous structures takes place by the formation of scar tissue which is less elastic and less functional than normal ligamentous tissue.”
“Sprains result in some degree of permanent injury.”
In this article, Dr. Jackson establishes the pathophysiological basis for manual therapy. She states:
“Any injury of the disc causes a disturbance in the dynamics of the motor unit of which the disc is a part. This leads to degeneration of the disc and the proximate joints.”
“Disturbances in the dynamics of the motor unit” is classic terminology for the chiropractic subluxation complex. The primary goal for manual manipulative therapy (adjustment) is to improve the motor unit functional disturbance.
Additionally, Dr. Jackson notes that traumatic inflammation “leads to post-traumatic fibrosis and adhesions.” Both fibrosis and adhesions are mechanical lesions that impair motion and function. Chiropractic manual manipulative adjustive approaches have been shown to benefit these mechanical lesions.
••••
The greatest achievement of Dr. Ruth Jackson’s incredible life is the publication of her book The Cervical Syndrome. The fourth and final edition of this book was published in 1978. The text is 399 pages in length and contains 158 Figures. The majority of these Figures involve sequential series of radiography showing the acceleration of degenerative joint disease as a time consequence of sustaining a cervical spine trauma.
When this book was reviewed by the Journal of the American Medical Association, it stated:
“This valuable book should be useful to the general practitioner, orthopedist, and neurosurgeon.”
The back cover of this book states:
“Treatment methods are dealt with in the final portion of the text. This section stresses more fully the importance of prevention and updates its reportage of proven therapeutic techniques. Nonsurgical treatment modalities covered span a wide area, from heat to massage, to traction, the cervical contour pillow and drugs, as well as exercises and manipulation.”
“Residents and practitioners in orthopaedics, of course, will want to take advantage of the knowledge presented in this outstanding text. It will also be useful to neurologists, radiologists, physical medicine and rehabilitation specialists, and general practitioners. Chiropractors and osteopathic physicians will find a wealth of information applicable to their practices.”
In this text, Dr. Jackson once again established the pathophysiological basis for manual manipulative therapy. She states:
“Healing occurs by the formation of scar tissue, which is less elastic and less functional than normal ligamentous tissue.”
“Immobilization of joints or functional inactivity results in stasis of circulation and is a common cause of posttraumatic joint stiffness. A small amount of movement in injured joints, rather than complete immobilization, reduces inflammation by mobilizing or dispersing the tissue breakdown products from the site of injury and prevents to some extent fibrous arthrosis.”
In the treatment section of her book, Dr. Jackson advocates many approaches and options, including heat and/or cold, massage, traction, postural correction, a cervical contour pillow to restore cervical lordosis during healing, vitamin C to aid healing, postural advice (while sleeping, working, reading, writing, driving, sitting, shaving, drinking), exercise, and manipulation. Pertaining to manipulation, Dr. Jackson states:
“Joint dysfunction is the result of loss of movement which is involuntary, and that movement can only be restored by being reproduced by the manipulator who restores normal function by the use of normal movement. There are many manipulators who manipulate the cervical spine and who claim excellent results.”
“Manipulation of the cervical spine should not be undertaken by any person who is not well versed in the anatomy of this very complex structure.”
Of course, chiropractors agree with these statements by Dr. Jackson. Chiropractors contend that their manipulative approach to joint problems is essential to restore normal function and movement when an involuntary loss of normal motion exists. Chiropractors study four years of anatomy, mechanics, orthopedics, neurology, radiology, clinical coaching as well as clinical applications to identify and safely manage these types of joint dysfunctional problems.
Dr. Jackson concludes that with proper treatment, most patient’s symptoms will subside within a period of three to six months. She also acknowledges that no two patients will respond exactly the same, and that “some treatment may be necessary in some cases over a longer period of time.”
References
1) R. M. and L. R., editors, Journal of Bone and Joint Surgery (American), RUTH JACKSON, M.D.: 1902-1994; VOL. 77-A, NO. 2. February 1995, pp. 331.
2) Jackson R, The Cervical Syndrome, Thomas, 1978.
3) Zillmer DA; Ruth Jackson, M.D.: A Woman of Determination and Accomplishment; The Iowa Orthopaedic Journal; Volume 21, 2001.