Low back pain (LBP) can be localized and contained to only the low back area or it can radiate pain down the leg. This distinction is important as the former, LBP only, is often less complicated and carries a more favorable prognosis for complete recovery. In fact, a large part of the history and examination when you seek treatment for back pain is focused on this differentiation. This month’s article will look at the different types of leg pain that can occur with different LBP conditions.
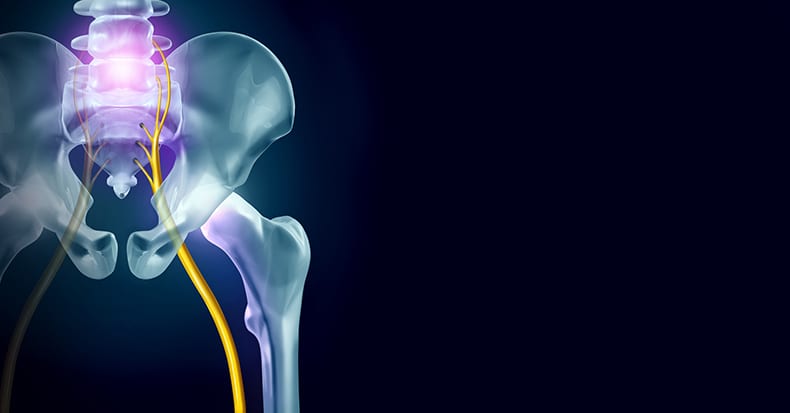
We’ve all heard of the word “sciatica” and it (usually) is loosely used to describe everything from LBP arising from the joints in the back, from the sacroiliac joint, from the muscles of the low back, and even from a pinched nerve caused by a ruptured disk. Strictly speaking, the term “sciatica” should ONLY be used when the sciatic nerve is pinched. The sciatic nerve is made up of five smaller nerves (L4, L5, S1, S2, S3) that arise from the spine and join together to form one large nerve (about the size of our pinky) called the sciatic nerve – like five small rivers merging into one BIG river. Sciatica occurs when any one of the small nerves (L4-S3) or when the sciatic nerve itself becomes compressed or irritated. This can be (and often is) caused from a lumbar disk herniation (the “ruptured disk”), a mis-positioned vertebra (such as a forward slip of the vertebra called “spondylolisthesis”), pressure from an arthritic spur off the spine where the nerve exits (“spinal stenosis”), or from a tumor near or around the nerve. A term called “pseudosciatica” (a non-disk cause) includes a pinch from the piriformis muscle where the nerve passes through the pelvis (in the “cheek” or the buttocks), which has been commonly referred to as “wallet sciatica” as sitting on the wallet in the back pocket is often the cause. When this occurs, the term “peripheral neuropathy” is the most accurate term to use. Other “pseudosciatic” causes include referred pain from the facet joints which is described by the patient as a “deep ache” inside the leg or from a metabolic condition where the nerve is affected by diabetes or other conditions. Here, the term “neuropathy” is the better label when diabetes, hypothyroid, lead poisoning, alcohol toxicity, and/or another cause is the culprit. Direct trauma, like a bruise to the buttocks from falling or hitting the nerve during an injection into the buttocks, can also trigger “sciatica.”
The symptoms of sciatica include low back pain, buttocks pain, back of the thigh, calf, and/or foot pain and/or numbness-tingling. If the nerve is compressed enough, muscle weakness can occur making it hard to stand up on the tip toes creating a limp when walking. In the clinic, your doctor may raise your straightened leg and if there’s a pinched nerve, then sharp pain can occur as the nerve is stretched. If pain occurs anywhere between 30 and 70° of elevation of either the same side leg and/or the opposite leg, this constitutes a positive test for sciatica (better termed, “nerve root tension”). When a disk is herniated into the nerve, bending the spine backwards can move the disk away and off the nerve resulting in relief, which is very diagnostic of a herniated disk. Having a patient walk on their toes and then heels and watching for foot drop as well as testing the reflexes, the sensation with a sharp object, and testing the reflexes at the knee and Achilles tendon can give your doctor clues if there is nerve damage. The GOOD NEWS is that chiropractic methods can resolve this problem, thus helping you to avoid unnecessary surgery! So, check with your doctor of chiropractic FIRST, before electing for surgery!!!