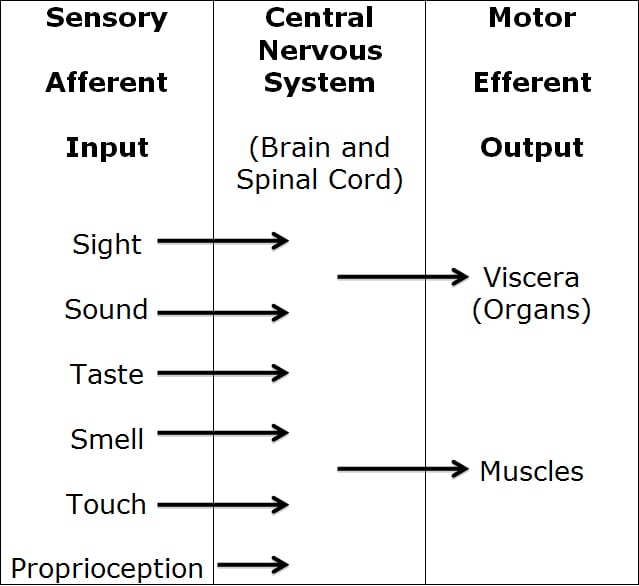
The nervous system can be categorized in many different ways. In understanding nervous system physiology, a simple but accurate way of categorization is to view the nervous system as two separate but integrated systems:
- The MOTOR nerve system
- The SENSORY nerve system
The MOTOR nerve system is the nerves that move our muscles (motor), and also control the function of our visceral organs (like heart, lungs, intestines, pancreas, liver, kidneys, etc.). The nerves that send the electrical signal from our brain and spinal cord to our muscles to control their contraction are actually called motor nerves. The nerves that send the electrical signal from our brain and spinal cord to control the function of our visceral organs are called autonomic nerves. This is because they function automatically, without our thinking and even when we are sleeping. Occasionally these autonomic visceral organ nerves are called visceral motor nerves. The motor nerve systems are output nerves, also called efferent nerves.
The SENSORY nerve system is the nerves that send electrical nerve signals into our spinal cord and brain. Therefore, the sensory nerves travel in the opposite direction of the motor nerves. The sensory nerve systems are input nerves, also called afferent nerves.
The sensory nerves have special endings (receptors) that can take environmental events, convert these events into an electrical signal, and send the electrical signal along sensory nerves to the brain for interpretation. The sensory nerves create our senses. It is our lifelong sensory experiences that “mold” our brain.
•••••
There are six primary sensory inputs into our brains:
- Sight (vision). Our eye has specific sensory receptors that have the ability to take specific electromagnetic waves in the environment, convert them into an electrical signal, send the electrical signal along a nerve (the optic nerve) to a specific place in the brain for interpretation (the occipital visual cortex).
- Sound (hearing). Similarly, the ear has specific sensory receptors that have the ability to take specific environmental disturbances, convert them into an electrical signal, send the electrical signal along a nerve (cochlear nerve) to a specific place in the brain for interpretation (the superior gyrus of the temporal lobe).
- Taste. When molecules from food or drink contact our tongue, again an electrical signal is sent via a sensory nerve to the brain for interpretation.
- Smell. When certain molecules in the air travel up our nose, an electrical signal is again sent via a sensory nerve to the brain for interpretation.
- Touch (requires sub categorization). There are special receptors on our skin and in other tissues like muscle, tongue, teeth, and viscera that generate an electrical single when they are mechanically perturbed. This electrical signal is once again sent via sensory nerves to the appropriate place in the brain for interpretation.
- Proprioception. Proprioception is often referred to as our “sixth” sense. There are special receptors in our skin, muscles, joints, fascia, etc., that generate an electrical signal that lets the brain know where we are in space. These receptors and their sensory nerves inform the brain about changes in the position and movements of the various parts of our bodies. Most of us know where our nose is, even when our eyes are closed, and we can easily touch our nose with the tip of our index finger (we also know where the tip of our finger is, even with eyes closed). With our eyes closed, we cannot see, hear, smell, taste, or touch our nose or fingertip, yet we can easily connect the two. This is proprioception.
Touch (#5) requires elaboration. Touch (for our purposes) will also include the sensations of pain and temperature (hot/cold). When there is a perturbation on our skin, we readily can distinguish between touch, pain, hot, and/or cold. All of these sensations are electrical signals that travel to various parts of the brain for interpretation.
The important point is that all perceptions (sight, sound, taste, smell, touch [including pain and temperature] and proprioception) occur in the cortical brain. “All perceptions are cortical.” This means that they occur in our brain. Lay people often believe that their eye sees, their ear hears, their tongue tastes, their nose smells, or that something at their toe or back or neck hurts. But actually these various parts of our body only initiate an electrical signal that is then interpreted in our brain.
•••••
The cortical perception of pain is a universal human experience. The electrical signal for the perception of pain in the brain is brought to the brain via special sensory nerves called nociceptive afferents or nociceptors.
All sensory inputs into the brain begin with a special receptor, except for pain (nociception). The receptor that initiates the electrical signal for sight is different than the receptor that initiates the electrical signal for sound or taste or smell. Pain (nociception) is the great receptor exception in that, for the most part, there is no receptor on the end of the nociceptive nerves. Consequently, the nociceptive nerve beginnings are referred to as free or naked receptors.
The pain problem in our country (USA) and in the world is astonishingly huge and it is getting worse. In the United States alone, 116 million Americans suffer from chronic daily pain (1). A recent cover article in the newspaper The Wall Street Journal quantifies the anatomical regions for American’s chronic pain (2):
Hip Pain 07.1%
Finger Pain 07.6%
Shoulder Pain 09.0%
Neck Pain 15.1%
Severe Headache 16.1%
Knee Pain 19.5%
Lower-Back Pain 28.1%
The total cost attributed to America’s pain problem, including treatment, lost productivity, and disability, is approaching $1 trillion per year.
It is useful to discuss pain using the categorizations of C. Chan Gunn, MD (3, 4). Dr. Gunn is a Clinical Professor at the Multidisciplinary Pain Center at the University of Washington Medical School, Seattle, Washington. Dr. Gunn’s pain categories are:
1) Nociception Pain
In this category of pain, there is no tissue damage, and therefore no inflammation. This is the type of pain one would experience if someone stepped on your toe; one would have pain but no tissue damage or inflammation. This type of pain does not require a healthcare provider to diagnose the cause of the pain. The cause of the pain is obvious; someone is standing on your toe.
Likewise, this type of pain does not require healthcare provider treatment. The treatment is obvious; get the person’s foot off your toe. The patient self treats.
With this type of pain, once the person’s foot is off your toe, you experience immediate and lasting relief. The prognosis is excellent.
This is the type of pain that most patients (and insurance companies) hope they are experiencing, hoping for instant relief. Sadly, this type of pain rarely makes it into a doctor’s office because it is self diagnosed and treated.
2) Algogenic Pain
Suppose that instead of someone stepping on your toe, they smacked your toe with a sledgehammer. Even though the hammer is no longer actually on your toe, your toe still hurts. The hammer added something to the equation, trauma, tissue damage, and inflammation. This disruption of the tissues and blood vessels by the trauma produces and releases inflammatory chemicals that are often collectively called algogenic exudates.
The inflammatory algogenic chemicals alter the thresholds of the nociceptive afferent system, increasing the pain electrical signal to the brain. Instant relief for this type of pain is not possible. The pain subsides as inflammation resolves and the nociceptive afferents system becomes sub-threshold.
Individuals suffering from this type of pain often go to healthcare providers for relief. Treatment often involves anti-inflammatory efforts (controlled motion, drugs, omega-3s, ice, electrical modalities, low–level laser therapy, etc.) and efforts to accelerate healing (low-level laser therapy). Depending upon the degree of tissue injury and a myriad of individual unique characteristics, response can last days, week, or months.
Chronic inflammation, caused by scar tissue, autoimmune responses, infection, etc., can cause chronic algogenic pain.
3) Neuropathic Pain
This is pain that persists after all possible tissue healing has occurred. Once again, instant relief for this type of pain is not possible. This is chronic pain that may persist for months, years, or forever.
•••••
Lay people often view pain solely as a bad thing, but healthcare professionals recognize pain to be both friend and foe. For example, if one sits on one’s foot for a prolonged period of time, it will eventually begin to hurt. This is an example of nociceptive pain. We simply self diagnose and treat our foot pain by moving it or changing our sitting position, and the pain goes away.
People are constantly doing things that begin to generate pain, and the pain afferents send a sensory signal to our brain reminding us to stop doing that activity. In this regard, pain keeps us safe, reminding us not to do certain things or to stop doing certain things. Without pain, we would not survive childhood and make it into adulthood.
Chronic pain is another story.
•••••
Of the many structures that make up the spine, most of them are capable of generating pain. All of the spinal structures that can initiate the pain signal to the brain have a common factor: they are innervated by sensory afferent nociceptive neurons that carry the pain electrical signal to the brain. As noted by exceptional spine care pioneer Alf Nachemson, MD, whatever causes spine pain must have a nerve (5). In 1991, Stephen Kuslich, MD, and colleagues clarified and quantified the spinal tissues that were capable of initiating the pain electrical signal to the brain as (6):
- Skin
- Superficial Muscles
- Deep Muscles
- Intervertebral Disc
- Facet Joint Capsules
- Periosteum of the Vertebral Bone
- Nerve roots
Any of these tissues are capable of initiating acute spinal pain. Chronic spinal pain perception was primarily attributed to the intervertebral disc and facet capsules, in that order (6). Other studies have primarily attributed chronic neck pain perception to the facet capsules and the intervertebral disc, in that reverse order (7).
•••••
For a new incidence of non-traumatic low back or neck pain, it is important for both clinicians and patients to make an initial quick assessment of the severity of the problem. Absent other historical indicators, it is common to assume the pain is algogenic in nature. This means there is an accumulation of algogenic inflammatory exudates that are increasing the sensitivity of the pain sensory nerves. The first step in doing this is to categorize the symptoms into one of three groups:
Group 1: Spinal pain alone
Either neck pain or back pain without pain radiation into the arms or legs. In general, algogenic spine pain that does not radiate is not serious. It is usually the consequence of a local inflammatory condition. It can be chronic and even disabling, but it is not dangerous.
Group 2: Sclerogenic pain; also known as sclerotomic pain or sclerotogenous pain
Sclerogenic pain radiates from the neck into the arm(s) or from the low back into the leg(s). Classically the pain radiation will not extend below the elbow (from the neck) or below the knee (from the low back).
As a rule, sclerogenic pain is difficult for the patient to localize. The pain presentation is often described as being deep and dull in character, similar to a toothache.
In general, sclerogenic pain is not dangerous. It is a form of referred pain that occurs as a consequence of a shared neuromere during embryonic development. In other words, the neurology of the back and the leg, or of the neck and the arm, are shared embryological, which can cause some confusion as to the exact location of the irritation when the electrical signal is sent to the brain. Originally based on the research of JH Kellgren and colleagues in 1938 and 1939, irritations of deep spinal tissues can cause sclerogenic pain referral to the arm or to the leg (8, 9).
In the sclerogenic pain patient, successful management of the deep spinal tissue irritations will resolve the sclerogenic pain referral. Deep spinal tissue irritations include irritations to the intervertebral disc, the facet joint capsules, and the core stabilization segmental mover muscles. These tissues respond excellently to spinal adjusting.
Group 3: Radicular pain, radiculitis, radiculopathy
The technical definition of radicular pain is that the spinal nerve root is inflamed, and the classic symptomatology is radiating arm or leg pain. In contrast to sclerogenic pain (a deep dull ache), the pain is often sharp and easily localized by the patient. Also, the pain often travels below the elbow (into the hands and fingers) and/or below the knee (into the foot and toes).
Radicular pain is more serious than sclerogenic pain. It is therefore a good idea to determine (to the best of one’s ability) if the pain is radicular or sclerogenic. History and physical examination can be quite accurate in establishing a differential diagnosis. However, conformation will require advanced diagnostic imaging. The current gold standard in advanced diagnostic imaging is magnetic resonance imaging, or MRI.
Radicular pain is often caused by compression of the nerve root, the compression causing nerve root irritation and/or inflammation. This pathology is commonly referred to as compressive radiculopathy. Interestingly, the compression itself is not necessarily painful. Rather, the pain arises when the compression initiates irritation and/or inflammation of the nerve root. The degree of nerve root compression and its seriousness is estimated with MRI scans.
The most classic cause of radicular compression is herniation of the intervertebral disc. Other causes include arthritic changes (degenerative joint disease, degenerative disc disease, spondylosis) causing osseous (bone spurs, hypertrophic changes, osteophytes) narrowing of the intervertebral foramen.
Each nerve root supplies a specific patch of skin (a dermatome) and a specific muscle (a myotome). Consequently, radicular compression is often associated with specific myotomal muscle weakness and altered sensation in the dermatomal patch of skin (paresthesias).
The deep tendon reflex is a common component of establishing if the extremity pain is sclerogenic or radicular. With radicular compression, the deep tendon reflex is diminished or possibly even absent. There are three common deep tendon reflexes in the arms (assessing the nerve roots of the neck), and two in the legs (assessing the nerve roots in the low back).
Radicular compressive pathology can result in permanent death of some of the neurons in the nerve root, resulting in permanent loss of various functions. Consequently, when compressive radiculopathyis suspected, “red flags” of such pathology should be watched for and assessed. These “red flags” include:
- Progressive myotomal muscle weakness.
- Atrophy of the muscle.
- Saddle anesthesia (loss of sensation in the area of the buttocks that would contact a saddle when sitting).
- Loss of bowel, bladder, and/or sexual function.(difficulty starting, difficulty ending, dripping, loss of sensation, etc.)
•••••
There are two (one for the neck and one for the low back) very simple tests that are commonly done by healthcare providers to help determine if radiating pain is sclerogenic referral or as a consequence of radicular compression. These tests can also be easily performed by patients to help determine the seriousness of compression and its progress while under treatment.
Both tests are stretch tests. If the nerve root is compressed, irritated, and inflamed as it exits the spinal column, stretching it will aggravate the discomfort and the radiation.
Low Back Pain With Leg Radiation Test
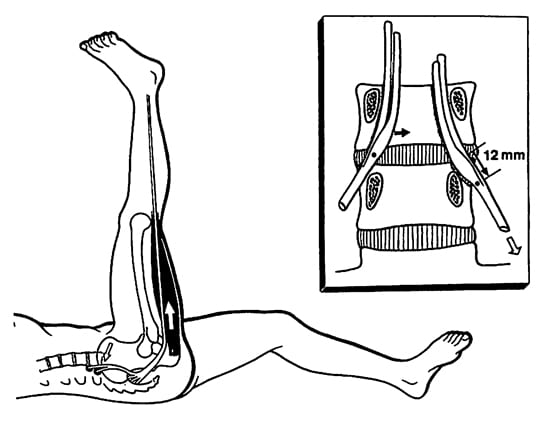
This test is known as the Straight Leg Raising Test. It is also known as Laseque’s Test, after Charles Laseque who first described the test in 1864 (10). The premise of the test is simple: movement of the leg causes movement of the lower lumbar nerve roots.
This test is performed by lying flat on one’s back and raising one’s leg up into the air while keeping the knee locked straight. Many normal people can do this to almost 90°. Individuals with lower back (lumbar) spinal radicular compressionwill begin to feel an increased in leg or back symptoms starting at about 35°.
According to Kapandji (11), when the leg is raised during the Straight Leg Raising Test, the lower lumbar spinal nerve roots will slide out of the nerve root hole (intervertebral foramen) by as much as half an inch (12 mm). If the nerve root is entrapped or compressed, the stretch will aggravate the irritation/inflammation, increasing symptoms.
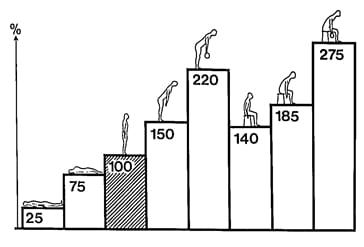
It is accepted that the primary cause of compressive radiculopathy is herniation of the intervertebral disc. Most patients with discogenic compressive radiculopathy obtain symptomatic relief when lying down flat on their back. The probable explanation for this is that the intradiscal pressure is least when in this position (12, 13)
In contrast, it is established that when one sits down, intradiscal pressures are increased by roughly a factor of 6 (25 psi to 140 psi) (12, 13).
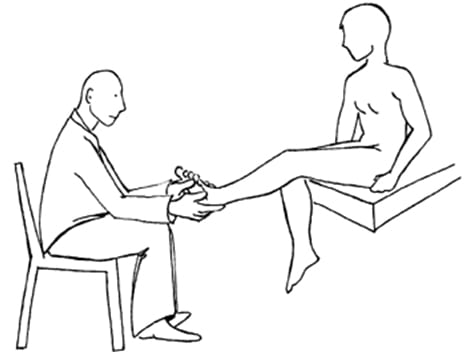
Therefore it is argued that performing the Straight Leg Raising Test when sitting down is a better indicator of the presence of discogenic compressive radiculopathy. This test is known as Bechterew’s Test. It is performed by sitting up straight, and then straightening out one’s leg until it is parallel with the horizon. An increase in leg or spinal symptomatology is considered to be a positive indicator of the presence of low back/leg compressive radiculopathy.
Brachial Plexus Tension Test of Elvey
The test that is an equivalent to the lower back Straight Leg Raising Test in the neck (cervical spine) is the Brachial Plexus Tension Test of Elvey. This test was originally described by Australian physiotherapist Robert Elvey in 1986 (14). Once again, the premise of the test is simple: movement of the arm causes movement of the lower cervical spine nerve roots.
The step-by-step procedure for performing the Brachial Plexus Tension Test of Elvey are well described by Quintner in the British Journal of Rheumatology in 1989 (15):
TO START:
Put the patient supine.
Externally rotate the arm and supinate the forearm.
Flex the fingers, wrist, and elbow.
Abduct the shoulder joint 110 degrees, so that the elbow is superior to the glenohumeral joint.
Put the arm behind the coronal plane of the body.
TO ASSESS:
Keep the shoulder girdle depressed.
Keep the forearm supinated.
Extend the elbow.
Extend the wrist, supination of the forearm.
Extend the fingers.
IF NEGATIVE:
Reassess with the head/neck laterally flexed to the opposite side.
Summary
Both cervical spine and lumbar spine compressive radiculopathies are coupled with a worse prognosis for complete recovery. Compressive radiculopathy typically requires more frequent treatment and more prolonged treatment. Compressive radiculopathy patients often have more long-term subjective and objective residuals, and more disability. Patients with compressive radiculopathy often require advanced imaging (such as MRI) for a full assessment of their pathology. Occasionally, patients with compressive radiculopathy will require a surgical decompression. These patients should always be monitored for the emergence of “red flag” signs.
The Straight Leg Raising Test (Laseque’s) and the Brachial Plexus Tension Test (Elvey) are simple tests to assess the presence of a compressive radiculopathic process.