Fibromyalgia Syndrome is the third most commonly diagnosed rheumatologic disorder, following osteoarthritis and rheumatoid arthritis. Fibromyalgia is characterized by widespread pain and tenderness, fatigue, morning stiffness, and sleep disturbance. Fibromyalgia is often disabling. Fibromyalgia is often treatment resistant. Fibromyalgia can be triggered by trauma (Greenfield, Waylonis, Buskila, Neumann). Studies report that between 25% and 50% of subjects with fibromyalgia recall physical trauma immediately prior to the onset of their symptoms (Al-Allaf).
Fibromyalgia Syndrome is diagnosed by identifying widespread pain and tenderness upon palpation at multiple anatomically defined soft tissue body sites. Fibromyalgia Syndrome overwhelmingly affects women more than men. “FM is nine times more common in middle-aged women (between the ages of 30 and 50 years) than in men (Abraham).”
THE GATE THEORY OF PAIN
In 1965, Ronald Melzack and Patrick Wall introduced the GATE THEORY OF PAIN. In 1985, orthopedic surgeon Kirkaldy-Willis published a pilot study of chiropractic spinal adjusting in the management of 283 patients suffering from chronic, treatment-resistant, low back pain. The results were excellent, essentially fixing 81% of the referred pain syndrome patients. Dr. Kirkaldy-Willis’ explanation for the positive clinical outcomes was based upon the fact that the improved motion would close the PAIN GATE.
Chiropractic management of patients with fibromyalgia syndrome traditionally involves the practical application of Melzack’s and Wall’s GATE THEORY OF PAIN. Chiropractic management of these patients involves improvement of the quality of mechanical neurological afferentation into the central nervous system in an effort to “close” the Pain Gate. Improving the sagittal and horizontal planes of spinal posture and motion through chiropractic is a proven method to “close” the pain gate, and has been so recognized at least since 1985 (Kirkalady-Willis). However, these mechanical efforts on those suffering from fibromyalgia syndrome may themselves worsen patient symptoms, at least temporarily, discouraging both patient and practitioner.
Consequently, chiropractors often utilize a number of adjunct approaches in the management of patients with fibromyalgia syndrome. Several of the adjunct approaches are reviewed below.
MALIC ACID and MAGNESIUM
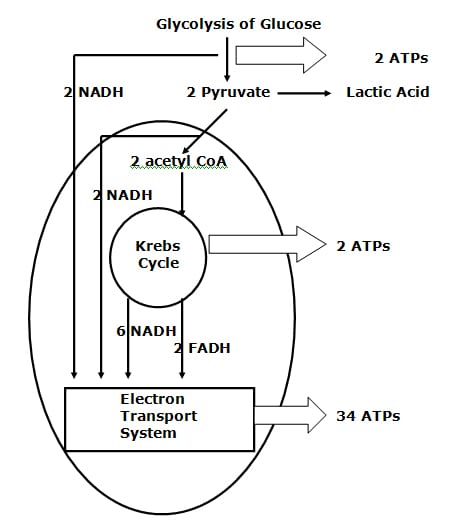
In 1992, Abraham and Flechas propose that fibromyalgia is caused by a deficiency of substances needed for ATP synthesis. The nociceptive nervous system requires a steady flow of ATP to remain at sub-action potential threshold. The nociceptive action potential is achieved primarily by an influx of positively charged Na+ ions. Keeping the potential across the membrane far away from excitation threshold is the job of the membrane-bound sodium pump, a mechanism that is ATP energy dependent. Reductions in ATP supplies could allow more Na+ ions to cross the membrane, bringing the nociceptive neuron much closer to excitation threshold. Trivial environmental stresses could now be sufficient to achieve nociceptive excitation and action potential, accounting for the widespread pain fibromyalgia patients experience.
During anaerobic glycolysis, from glucose to acetyl-Co A, there are 11 distinct steps; 9 of 11 steps (82%) require magnesium.
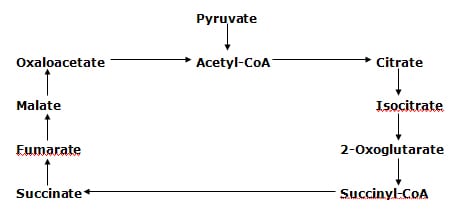
Central to ATP generation is the Krebs Cycle (Citric Acid Cycle). The Krebs Cycle has nine steps, and 3 of them require magnesium. The rate limiting Krebs Cycle step in the genesis of ATP is malic acid (malate). In humans, when there is increased demand for ATP, there is also an increased demand and utilization of malate and magnesium. Malate deficiency is the cause of the ATP deficiency seen with exhaustive physical activity.
Without adequate levels of malate and magnesium, there is increased anaerobic glycolysis, resulting in increased pyruvate production and increased lactic acid, both of which increase pain perception. Magnesium and malate have a critical role in ATP production, and therefore fibromyalgia symptoms may be caused by magnesium and malate deficiency.
Abraham and Flechas explain the synergistic role of magnesium and malic acid in the genesis of ATP. They detail the biochemistry of how reductions in magnesium and malic acid would result in ATP deficiency.
Abraham and Flechas then treat 15 fibromyalgia patients with daily 300-600 mg of magnesium plus 1200-2400 mg malic acid. “All patients reported significant subjective improvement of pain within 48 hours of starting” supplementation.
In 1995, Russell and colleagues, in a randomized, double blind, placebo controlled, crossover study, also used magnesium and malic acid to treat 29 patients with fibromyalgia, noting “significant reductions in the severity of all 3 primary pain/tenderness measures were observed.” Better results were observed in those taking 600 mg of magnesium and 2400 mg of malic acid, as compared to those who took lower doses. The authors note that this supplementation should continue for al least 2 months, and often for as long as 6 months.
THE SEROTONIN PATHWAY
In 2004, Borut Banic and colleagues, writing in the journal Neurology, presented extensive evidence suggesting that fibromyalgia is the consequence of reduced levels of the brain neurotransmitter serotonin.
In 1998, osteopath John H Juhl also proposed that fibromyalgia could be related to reduced serotonin. He notes that researchers have found low serum levels of serotonin in fibromyalgia patients. Low serum serotonin levels have been found to have an inverse correlation with clinical measures of pain.
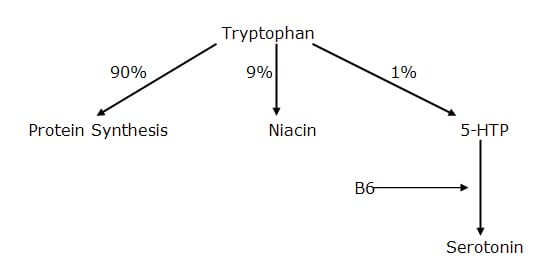
The serotonin pathway begins with the essential amino acid tryptophan. Tryptophan is the least common of the 8 essential amino acids, accounting for about 1% of protein content.
After absorption, about 90% of tryptophan is used at the peripheral tissues for protein synthesis.
About 9% of absorbed tryptophan is used to produce niacin. The RDA for niacin is 15 mg. It takes 60 mg of tryptophan to produce 1 mg of niacin. This is important, because if niacin levels are adequate in the diet, the body will not need to use this 9% to make niacin. In fact, the higher the dietary levels of niacin, the less tryptophan is converted to this pathway. This increases the tryptophan available to be converted to serotonin.
About 1% of absorbed tryptophan is converted to serotonin.
In the body, tryptophan is converted to 5-hydroxy-tryptophan
(5-HTP). 5-HTP easily crosses the blood-brain barrier for conversion to serotonin in the central nervous system. The conversion of 5-HTP to serotonin requires vitamin B6. Consequently, inadequate levels of B6 impair the conversion of tryptophan to serotonin.
Currently, tryptophan is available by prescription only in the United States. However, 5-HTP is sold, and as noted above, still crosses the blood brain barrier for conversion to serotonin, as does tryptophan. Commercially, 5-HTP is extracted from the seeds of Grifonia simplicifolia, a plant grown in West Africa.
Dr. Juhl notes 2 published studies where supplementation of 5-HTP in the dose of 100 mg 3 times per day in patients with fibromyalgia resulted in significant improvement of clinical symptoms after 30-90 days. The effective daily dose range appears to be 200-1000 mg per day, and that it should be taken with meals. These patients should also be given vitamin B6 to increase conversion of 5-HTP to serotonin, and niacinamide to inhibit the need for tryptophan to convert to niacin.
Dr. Rodger Murphree supports the tryptophan to 5HTP to serotonin pathway noted by Dr. Juhl. In his 2003 book titled Treating and beating Fibromyalgia and Chronic Fatigue Syndrome, Dr. Murphree suggests supplementing with 100-300 mg of 5HTP on an empty stomach 30 minutes before bed. He notes that it can take several nights to two weeks before 5HTP starts to work.
LOW LEVEL LASER THERAPY
Below are 3 studies that show significant benefit to management of chronic pain and fibromyalgia using low-level laser therapy. The first article is by Green, et al in 2000. The authors claim excellent positive therapeutic results in treating patients with chronic painful diabetic neuropathy, chronic myofascial pain, or complex regional pain syndrome.
Green et al conclude, “It appears that photon stimulation carries with it a significant potential for amelioration of chronic pain in which autonomic and neurovascular abnormalities are, in fact, present.”
The second article is a randomized controlled clinical trial done in 2002 by Gur et al on patients with fibromyalgia. The laser group of patients were treated for 3 minutes at each tender point daily for 2 weeks. The authors note “Significant improvements were indicated in all clinical parameters in the laser group,” and that “laser therapy can be used as a monotherapy or as a supplementary treatment to other therapeutic procedures in fibromyalgia.”
Gur and colleagues also published the third article in 2002 in the journal Lasers in Surgery and Medicine. It is a single-blinded placebo-controlled trial of low power laser therapy in 40 female patients with fibromyalgia. The authors note that there was a “significant difference was in parameters as pain, muscle spasm, morning stiffness and tender point numbers in favour of laser group.” These authors conclude “Our study suggests that laser therapy is effective on pain, muscle spasm, morning stiffness, and total tender point number in fibromyalgia and suggests that this therapy method is a safe and effective way of treatment in the cases with fibromyalgia.”
According to a book chapter titled “Low-Power Laser Therapy” by Tina Karu, low-level laser therapy physiologically increases the mitochondrial production on cellular energy ATP. This is similar to the proposed mechanism of supplementing with malic acid and magnesium, as noted above.
EXCITOTOXINS
Below are listed 5 books that deal extensively with dietary excitotoxins and their deleterious effects on human physiology. These deleterious effects include chronic fibromyalgia pain because dietary excitotoxins also function as excitatory neurotransmitters for chronic pain (Dickenson).
In short, dietary excitotoxins are added to food because they function as excitatory neurotransmitters, enhancing the flavor of food. The two main dietary excitotoxins are glutamate (often labeled monosodium glutamate or MSG, and aspartame because it is metabolized to the excitotoxin aspartate).
In excess, these substances can literally excite neurons to death, and therefore have been associated with neurodegenerative diseases such as Alzheimer and Parkinson diseases, as well as a plethora of other symptoms, including fibromyalgia chronic pain. Unfortunately, excitotoxins such as glutamate can have dozens of names on food labels.
In 2001, Smith reports on 4 cases of chronic pain fibromyalgia patients who where successfully treated after avoiding all products that contain the excitotoxins glutamate and aspartame. Some of these patients had suffered for as long as 17 years, and were taking as many as 13 different drugs for their symptoms.
Smith notes the following:
“Excitotoxins are molecules, such as MSG and aspartate that act as excitatory neurotransmitters, and can lead to neurotoxicity when used in excess.”
“MSG, the sodium salt of the amino acid glutamic acid or glutamate, is an additive used to enhance the flavor of certain foods.”
The US Food and Drug Administration (FDA) grandfathered MSG, like salt and baking powder, as harmless food substances in 1959.
Aspartame was first marketed in 1981, and is a dipeptide of aspartate and phenylalanine used in foods, beverages, and drugs.
“Anecdotally, aspartame use in humans has been linked with head aches, seizures, dizziness, movement disorders, urticaria, angioedema, and anaphylaxis.”
“Much of the research performed proving that glutamate was safe for human consumption may have been flawed.”
Glutamate has a role in chronic pain sensitization:
“MSG is nearly ubiquitous in processed food, appearing under many names, including gelatin, hydrolyzed vegetable protein, textured protein, and yeast extract.”
Aspartame is the dominant artificial sweetener on the market since 1981.
Fibromyalgia can be caused by exposure to dietary excitotoxins in susceptible individuals.
Aspartate and glutamate taken together have additive neurotoxic effects.
The elimination of MSG and other excitotoxins from the diets of patients with fibromyalgia offers a benign treatment option that has the potential for dramatic results in a subset of patients.
There are dozens of names for glutamate as it is added to foods. A partial list of names seen on food packaging are listed below, from the website www.truthinlabeling.org
HIDDEN SOURCES OF PROCESSED FREE GLUTAMIC ACID (MSG)
NAMES OF INGREDIENTS THAT CONTAIN ENOUGH MSG TO SERVE AS COMMON MSG-REACTION TRIGGERS
These ALWAYS contain MSG
Glutamate Glutamic acid Gelatin
Monosodium glutamate Calcium caseinate Textured protein
Monopotassium glutamate Sodium caseinate Yeast nutrient
Yeast extract Yeast food Autolyzed yeast
Hydrolyzed protein (any protein that is hydrolyzed) Hydrolyzed corn gluten
These OFTEN contain MSG or create MSG during processing
Carrageenan Maltodextrin Malt extract
Natural pork flavoring Soy protein isolate Malt flavoring
Bouillon and Broth Natural chicken flavoring Citric acid
Natural beef flavoring Ultra-pasteurized Soy sauce Stock Barley malt
Soy sauce extract Whey protein concentrate Pectin
Anything fermented Whey protein Protease
Soy protein concentrate Whey protein isolate Protease enzyme Anything protein fortified Flavors(s) & Flavoring(s) Soy protein
Anything enzyme modified Enzymes anything Seasonings
Natural flavor & flavoring
The website further notes that “The new game is to label hydrolyzed proteins as pea protein, whey protein, corn protein, etc. If a pea, for example, were whole, it would be identified as a pea. Calling an ingredient pea protein indicates that the pea has been hydrolyzed, at least in part, and that processed free glutamic acid (MSG) is present.”
“Low fat and no fat milk products often include milk solids that contain MSG. Drinks, candy, and chewing gum are potential sources of hidden MSG and of aspartame and neotame.”
“Aspartic acid, found in neotame and aspartame (NutraSweet), ordinarily causes MSG type reactions in MSG sensitive people. Aspartame is found in some medications, including children’s medications.”
EXERCISE
The majority of fibromyalgia patients are aerobically unfit and have poor muscle strength and limited flexibility. A number of studies have shown that exercise improves the clinical status of fibromyalgia patients. As an example, in 2007, Bircan and colleagues published a study in which fibromyalgia patients were assigned to either treadmill (aerobic) exercise or weight lifting exercise. In both groups, the exercises were initially at a lower level of intensity; the intensity was increased in subsequent exercise sessions based on patient tolerance. No patient experienced musculoskeletal injury or exacerbation of fibromyalgia-related symptoms during either exercise intervention. The authors documented that both exercise groups were “effective at improving symptoms, tender point count, fitness, psychological status and quality of life in fibromyalgia patients.” Interestingly, they also found that muscle strengthening exercise was superior to aerobic training in improving the fitness in fibromyalgia patients.
This month (November 2010), Carson and colleagues published a study in the journal Pain evaluating the effects of an 8-week yoga program on 53 women diagnosed with Fibromyalgia Syndrome. The program showed these women experienced significant improvement in all aspects of their symptoms and function.
OMEGA-3 FATTY ACIDS
A number of studies have shown that the omega-3 fatty acid eicosapentaenoic acid (EPA) is effective in the management of pain syndromes. Probably the article most referenced in this regard is the one authored by the neurosurgeon for the Pittsburgh Steeler football team, Dr. Joseph Maroon, in the journal Surgical Neurology, 2006. Dr. Maroon explains how EPA inhibits the cascade of the omega-6 fatty acid arachidonic acid into the pro-inflammatory eicosanoid hormone prostaglandin E2.
In his 2002 book The Omega Zone, biochemist Barry Sears reports that he is able to completely eliminate fibromyalgia symptoms by administering 18 grams (18,000 mg) of fish oil. He notes that his fish oil formula contained twice as much eicosapentaenoic acid (EPA) as docosahexaenoic acid (DHA).
This year (2010), Ko and colleagues published a study on patients with neuropathic pain syndrome, of which they included Fibromyalgia Syndrome. They reported excellent clinical outcomes with the administration of 2,400-7,500 mg of fish oil supplementation (EPA + DHA) per day.
FIBROMYALGIA SYNDROME AND WHIPLASH TRAUMA
As noted above, a number of studies have linked Fibromyalgia Syndrome to physical trauma, including whiplash injury.
In their 1992 book, Painful Cervical Trauma, Diagnosis and Rehabilitative Treatment of Neuromusculoskeletal Injuries, C. David Tollison and John Satterthwaite state:
“A particularly frustrating group of patients are those with a typical whiplash injury who, rather than gradually improving, actually seem to progressively develop a generalized chronic pain state identical to the fibromyalgia syndrome.”
Tollison and Satterthwaite state that fibromyalgia follows trauma approximately 22% of fibromyalgia patients.
In 1992, Greenfield and colleagues reviewed 127 cases of fibromyalgia and determined that 23% were triggered by a traumatic event. They also noted that patients suffering from trauma fibromyalgia were more disabled than those suffering from primary (non-traumatic) fibromyalgia.
In 1994, Waylonis and Perkins evaluated 176 patients who had been suffering from post-traumatic fibromyalgia. The traumatic cause was determined to be whiplash injury in 61% of the subjects. Years after the initial diagnosis, “eighty-five percent of the patients continued to have significant symptoms and clinical evidence of fibromyalgia.
In 1997, Buskila and colleagues studied the relationship between cervical spine injury and the development of fibromyalgia syndrome. They assessed 102 patients with neck injury and a control group of 59 patients with leg fracture. Twenty-two percent of the neck injury patients developed fibromyalgia, while only 1.7% of those with leg fracture developed fibromyalgia. The authors concluded “fibromyalgia syndrome was 15 times more frequent following neck injury than following lower extremity injury.”
In 2002, Al-Allaf and colleagues stated that 25% to 50% of those with Fibromyalgia Syndrome have physical trauma immediately prior the onset.
In 2003, Neumann and colleagues evaluated the outcomes of 78 post-traumatic neck injury fibromyalgia cases. They determined that 60% were still suffering from their fibromyalgia symptoms at the three-year follow-up. They also determined that nearly all of the persistently symptomatic patients were women, indicating that whiplash fibromyalgia recovery is worse in women than men.
In 2005, Samuel McLean and colleagues from the University of Michigan Medical Center established the criteria to assign fibromyalgia to whiplash trauma. They state:
“To summarize, there are abundant data suggesting that it is biologically plausible that physical trauma, acting as a stressor, could lead to the development of chronic widespread pain, as well as a number of other somatic symptoms.”
“Using these above attribution elements, the association between fibromyalgia and motor vehicle collision meets criteria one (temporal association), two (lack of alternative explanations), three (biological plausibility), six (analogy), and possibly five (re-challenge). This meets or exceeds the recommended threshold for suspecting a causal relationship between an exposure and subsequent illness. To put the relationship between fibromyalgia and trauma in context, there are at least as much data supporting this relationship as there are for many other accepted environmentally associated rheumatic diseases.”
“Thus, trauma may be only one of many types of stressors capable of producing symptoms characteristic of fibromyalgia.”
SUMMARY
Fibromyalgia patients are often quite resistant to traditional treatment approaches. Today’s chiropractors use all or some of the above adjuncts, along with traditional joint adjusting, tissue work, postural improvement and exercise. Most patients so treated experience substantial benefit and achieve acceptable clinical improvement. Whiplash-injured patients are treated identically to fibromyalgia cases that are of a non-traumatic origin. It should be understood that whiplash-injured patients who develop fibromyalgia would require more treatment and a longer course of treatment than other whiplash-injured patients. Because fibromyalgia syndrome patients are often treatment resistant, the prognosis for complete recovery is guarded.
REFERENCES
Abraham GE, Flechas JD. Management of Fibromyalgia: Rationale for the Use of Magnesium and Malic Acid. J of Nutritional Med. 1992 (3) 49-59.
Al-Allaf AW, Dunbar KL, Hallum NS, Nosratzadeh B, Templeton KD, Pullar T. A case–control study examining the role of physical trauma in the onset of fibromyalgia syndrome; Rheumatology 2002; 41: 450-453.
Bircan C, SKarasel SA, Akgün B, El O, Alper S; Effects of muscle strengthening versus aerobic exercise program in fibromyalgia; Rheumatology International; November 3, 2007.
Borut Banic, Steen Petersen-Felix, Ole K. Andersen, Bogdan P. Radanov, P. M. Villiger, Lars Arendt-Nielse and Michele Curatolo. Evidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgia. Pain. January 2004, Pages 7-15.
Buskila D, Neumann L, Vaisberg G, Alkalay D, Wolfe F. Increased rates of fibromyalgia following cervical spine injury. A controlled study of 161 cases of traumatic injury. Arthritis Rheum. 1997 Mar;40(3):446-52.
Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010 Nov;151(2):530-9.
Dickenson AH. Gate Control Theory of pain stands the test of time British Journal of Anaesthesia, Vol. 88, No. 6, June 2002, Pgs. 755-757.
Green J, Fralicker D, Clewell W, Horowitz E, Lucey T, Yannacone V, Haber C. INFRARED PHOTON STIMULATION: A NEW FORM OF CHRONIC PAIN THERAPY. American Journal of Pain Management, Vol. 10, No. 3 July 2000,113-120;
Greenfield S, Fitzcharles MA, Esdaile JM. Reactive fibromyalgia syndrome. Arthritis Rheum. 1992 Jun;35(6):678-81.
Gur A, Karakoc M, Nas K, Cevik R, Sarac J, Ataoglu S. Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int. 2002 Sep;22(5):188-93.
Gur A, Karakoc M, Nas K, Cevik R, Sarac J, Demir E. Efficacy of low power laser therapy in fibromyalgia: a single-blind, placebo-controlled trial. Lasers Med Sci. 2002;17(1):57-61.
Juhl JH, (1998-10-01). “Fibromyalgia and the serotonin pathway”, Altern Med Rev;3(5):367-75.
Karu, Tina, “Low-Power Laser Therapy”, Chapter 48 in Biomedical Photonics Handbook, Tuan Vo-Dinh, CRS Press, 2003.
Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985, Vol. 31, pp. 535-540.
Ko GD, Nowacki NB, Arseneau L, Eitel M, Hum A; Omega-3 Fatty Acids for Neuropathic Pain: Case Series; The Clinical Journal of Pain; February 2010, Vol. 26, No, 2, pp 168-172.
Maroon JC, Bost JW; Omega-3 Fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain; Surgical Neurology; 65 (April 2006) 326– 331.
Melzack R, Wall PD; Pain Mechanisms: A New Theory; Science; November 19, 1965’ 150(699): pp. 971-9.
McLean SA, Williams DA Clauw DJ; Fibromyalgia After Motor Vehicle Collision: Evidence and Implications; Traffic Injury Prevention, 2005; No. 6, pp. 97–104.
Murphree, Rodger, Treating and beating Fibromyalgia and Chronic Fatigue Syndrome, The Definitive Guide for Patients and Physicians, Harrison and Hampton Publishing, 2003.
Neumann L, Zeldets V, Bolotin A, Buskila D. Outcome of posttraumatic fibromyalgia: A 3-year follow-up of 78 cases of cervical spine injuries.
Semin Arthritis Rheum. 2003 Apr;32(5):320-5.
Russell IJ, Michalek JE, Flechas JD, Abraham GE. Treatment of fibromyalgia syndrome with Super Malic: a randomized, double blind, placebo controlled, crossover pilot study. J Rheumatol. 1995 May;22(5):953-8.
Sears B; The Omega Zone, Regan Books, 2002.
Smith JD, Terpening CM, Schmidt SOF, Gums JG. Relief of Fibromyalgia Symptoms Following Discontinuation of Dietary Excitotoxins The Annals of Pharmacotherapy: Vol. 35, No. 6, pp. 702–706. June 2001
Tollison CD, Satterthwaite JR; Painful Cervical Trauma, Diagnosis and Rehabilitative Treatment of
Neuromusculoskeletal Injuries, Williams & Wilkins, 1992. Waylonis GW, Perkins RH. Post-traumatic fibromyalgia. A long-term follow-up. Am J Phys Med Rehabil. 1994 Nov-Dec;73(6)