Soccer’s World Cup, 2010, has just finished. Having watched many of the games, I constantly observed players “head” the ball, and often the ball had traveled more than half the length of the playing field prior to contacting the head while “on the fly.”
In 2004, researchers from Cankaya University, Ankara, Turkey, published an article in the European Spine Journal, titled (1):
Soccer causes degenerative changes in the cervical spine
In this study, the authors assessed the incidence of degenerative changes of the cervical spine joints in active amateur and veteran soccer players. They designed a cross-sectional descriptive study using biomechanical, radiological, and magnetic resonance assessments. The study subjects were active (<30 years; n=15) and veteran (>30 years; n=15) male amateur soccer players, and their age-matched controls (n=13 and n=15).
The authors found that degenerative changes were prominent in veteran players, and the sagittal diameter of their spinal canal at C2 to C6 was lower when compared to controls. Narrowing of the sagittal spinal canal diameter suggests advancing degenerative spondylotic changes, predisposing these individuals to spinal cord myelopathy. Consequently, magnetic resonance findings of degeneration were more prominent in soccer players when compared to their age-matched controls. These authors note:
“Severe muscle spasms, spinal cord injuries, disc herniation and fracture dislocations are documented among the acute injuries to the cervical spine in soccer.”
In soccer, “scoring, defending and passing the ball with the head is an integral part of this game; so chronic degenerative changes should be common in the cervical spine.”
“High- and/or low-impact recurrent trauma mainly due to heading the ball may initiate degenerative changes at the cervical spine.”
“The cervical spine absorbs a significant amount of the force generated due to heading the ball. This type of repetitive force during competition or training may increase the risk of degeneration at the intervertebral joints, intervertebral discs or the spinal cord.”
“Continuous micro- and macro-trauma to the cervical spine due to heading the ball in soccer may cause early degenerative changes.”
“Cervical disc bulging, osteophytes in the cervical canal, disc protrusion, loss of cervical lordosis, spinal cord compression, and cord compression in hyperflexion were the most common MR findings.”
The “degenerative changes of the cervical spine in soccer are not only limited to the skeletal tissues but may also extend to the soft tissues, including the intervertebral disc and the spinal cord.”
“Biomechanical, radiological, and MR findings present a tendency towards early degenerative changes of the cervical spine most probably due to heading the ball in soccer.”
“A tendency towards early degenerative changes exists in soccer players most probably due to high- and/or low-impact recurrent trauma to the cervical spine caused by heading the ball.”
“The onset of such [spinal degenerative] changes was 10–20 years earlier than that of the normal population.”
•••••
There is an important difference between soccer cervical spine trauma and whiplash injury cervical spine trauma. Clearly, “heading” the soccer ball is primarily a repeated microtraumatic event; an event that occurs hundreds or thousands of times over years or decades. In contrast, whiplash injury is usually a single macrotraumatic event. These questions are explored in this work:
1) Do whiplash injury single macrotraumatic events lead to the acceleration of cervical spine degeneration and arthritis (spondylosis)?
2) What is the relationship between whiplash trauma and reversal of the normal cervical lordotic curve, or cervical spine kyphosis?
3) Does cervical spine kyphosis accelerate cervical spine spondylosis and cervical spinal cord dysfunction (myelopathy)?
4) Is there any evidence that cervical spine kyphotic deformity can be improved or corrected with chiropractic management?
I will explore these questions one at a time.
1
Do whiplash injury single macrotraumatic events lead to the acceleration of cervical spine degeneration and arthritis (spondylosis)?
In 1964, whiplash injury expert and pioneer, Ruth Jackson, MD, from Baylor University Medical School, published an article in the American Journal of Orthopedics titled (2):
“The Positive Findings In Neck Injuries”
Dr. Jackson’s conclusions in this article were based on her evaluation of 5,000 injured patients. She notes:
“An adequate radiographic examination of the cervical spine is essential for diagnosis.”
“Any injury of the disc causes a disturbance in the dynamics of the motor unit of which the disc is a part. This leads to degeneration of the disc and the proximate joints.”
•
The 1989 reference text produced by the Cervical Spine Research Society titled (3):
The Cervical Spine Research Society
addresses the question of whiplash trauma and acceleration of degenerative disc disease. The text notes that in one study, x-rays taken an average of 7 years after whiplash injury showed neck disc arthritis was present in 39% of the patients. The control group only showed a neck disc arthritis incidence of 6%. The authors concluded:
“Thus, it appeared that the injury had started the slow process of disc degeneration.”
•
In 1993, Dr. Hamer and colleagues published a study pertaining to whiplash injury and surgical cervical disc pathology. The study was published in the journal Injury and titled (4):
Whiplash injury and surgically treated cervical disc disease
In this study, the authors reviewed the incidence of a previous whiplash injury in 215 patients who underwent an anterior cervical discectomy and fusion. The rate of this disc surgery was found to be twice that of a control population of 800 general orthopaedic outpatients. The mean age at which the whiplash injury occurred in the surgical group was 37 years and in the control group 36 years. The mean age at operation of those patients with a previous whiplash injury (45 +/- 12 years) was significantly less than those patients without a previous whiplash injury (55 +/- 14 years). These authors concluded:
“This study provides further evidence that whiplash injury causes structural changes predisposing to premature degenerative disc disease.”
•
In 1997, Drs. Gargan and Bannister published a long-term follow-up comparison study of whiplash-injured patients to a group of matched controls. This study appeared in the Journal of Orthopedic Medicine, titled (5):
The Comparative Effects of Whiplash Injuries
This study is a cross-sectional age and sex-matched comparison of the clinical signs and radiographic features of 41 patients 10 years after whiplash injury, with 80 clinical and 100 radiographic controls. Specifically, the symptoms and signs of 41 patients who had sustained a whiplash injury 10 years previously were compared with 80 age-matched controls and their radiographs with 100 age-matched controls. Importantly, the x-rays showed that radiographic degenerative changes in the cervical spine appeared 10 years earlier in the whiplash group than in the control group, leading Gargan and Bannister to conclude:
“The prevalence of degenerative changes in the younger cervical spine [of the whiplash group] suggests that the condition has an organic basis.”
“After soft tissue neck trauma, degenerative change presented over 4 times as frequently in those aged between 31 and 40 and twice as often between 41 and 50.”
“Degenerative change and its association with neck stiffness support an organic basis for the symptoms that follow soft tissue injuries of the neck.”
•
These studies indicate that whiplash trauma does in fact initiate and
accelerate degenerative changes of the cervical spine, spondylosis.
2
What is the relationship between whiplash trauma and reversal of the normal cervical lordotic curve, or cervical spine kyphosis?
The greatest achievement of Dr. Ruth Jackson’s remarkable life is the publication of her book The Cervical Syndrome (6). The fourth and final edition of this book was published in 1978. The text is 399 pages in length and contains 158 figures. The majority of these figures involve sequential series of x-rays showing the acceleration of degenerative joint disease as a consequence of time after sustaining a cervical spine trauma. A common denominator in these series includes kyphotic angulation of the cervical spine following whiplash injury; when these kyphotic angulations are radiographically followed over a period of years, there is a predictable pattern of acceleration of cervical spondylosis observed. Dr. Jackson states:
“A loss of the forward curve which can be noted in the lateral view made with the patient looking straight ahead is indicative of some disorder of the cervical spine.”
“Loss of the forward curve occurs in 78% of all cases of cervical involvement and a reversal of the forward curve [kyphosis], which is localized usually to 3 or 4 segments, will be found in 20% of these cases. The apex of the reversed curve indicates usually the site of maximum involvement.”
“The reversed curve may present a sharp angulation at one specific level. This indicates a tearing of the posterior ligamentous structures or a rupture of the intervertebral disc anteriorly at that level. Subluxation of the posterior joints upward and forward with widening of the posterior joint spaces and separation of the corresponding spinous processes may be responsible, also, for the posterior angulation.”
Dr. Jackson discourages sleeping on the back with a regular pillow because it places the cervical spine in a position of kyphosis. She advocates the use of a “Cervical Contour Pillow” which maintains a normal cervical lordosis. Her text has photographs of radiographs of patients with both a normal pillow and the contour pillow to support her point.
•
Radiologist Lee Hadley, MD, in his 1979 text Anatomico-Roentgenographic Studies of the Spine, also shows several long-term case studies of cervical kyphosis progression to cervical spondylosis (7). On page 135 of his text, he states that cervical kyphotic angulation “should be considered a permanent injury.”
•
In 1995, radiologist Dr. Harry Griffiths and colleagues from the Department of Radiology, University of Minnesota Hospital, published an article in the journal Skeletal Radiology, titled (8):
Hyperextension strain or “whiplash” injuries to the cervical spine
In this study, the authors evaluated a full cervical spine radiographic series in 40 patients with clinically proven whiplash injuries and compared them to the radiographs of 105 normal controls. They found that patients with cervical kyphosis of greater than 10 degrees occurred in the whiplash-injured group 80%. They suggested that this finding was indicative of a more severe ligamentous injury at the segmental level below the kyphotic angulation.
•
In 2002, the journal Emergency Radiology published a study titled (9):
The use of flexion and extension MR in the evaluation
of cervical spine trauma: initial experience in 100 trauma patients compared with 100 normal subjects
In this study, the authors evaluated the cervical spines of 100 consecutive uninjured normal asymptomatic adults and 100 adult accident victims following rear-end low-impact motor vehicle accidents using rapid T2-weighted MRI. The injured subjects were evaluated during the subacute period, at 12 to 14 weeks after injury, following clinically resolved muscle spasm.
In the control, population, loss of normal cervical lordosis was observed in 4% of the subjects. In the subacute whiplash-injured patient population, loss of cervical lordosis was observed in 98% of the group. The authors were unable to ascribe this finding to muscle spasm.
•
These studies clearly indicate that cervical spine kyphosis certainly can occur as a consequence of whiplash trauma. They also indicate that cervical kyphosis is significantly more likely to be found in a whiplash patient population than in controls. Additionally, these cervical spine kyphotic deformities in whiplash-injured patients are unlikely to be caused by muscle spasm; rather they are much more likely to be the result of more significant ligamentous injury.
3
Does cervical spine kyphosis accelerate cervical spine spondylosis and cervical spinal cord dysfunction (myelopathy)?
In 2001, researchers from the Department of Orthopaedic Surgery, Shiga University of Medical Science, Otsu, Japan, published a study in the European Spine Journal titled (10):
Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels
In this study, 42 patients who underwent anterior interbody fusion surgery for cervical spondylosis and disc herniation were followed for an average of 9.8 years. The authors found degenerative change in adjacent intervertebral levels was observed in 77% of the fused segment when there was kyphotic angulation, which was statistically significant. They stated:
“Our findings suggest that one of the factors promoting degenerative change in adjacent intervertebral levels after anterior cervical fusion for degenerative disorders is postoperative kyphotic change in the cervical spine.”
•
In 2007, researchers from the Departments of Neurosurgery and Radiology, Dokuz Eylul University, Izmir, Turkey, published an article in the Journal of Spinal Disorders & Techniques, titled (11):
Kyphosis One Level Above the Cervical Disc Disease:
Is the Kyphosis Cause or Effect?
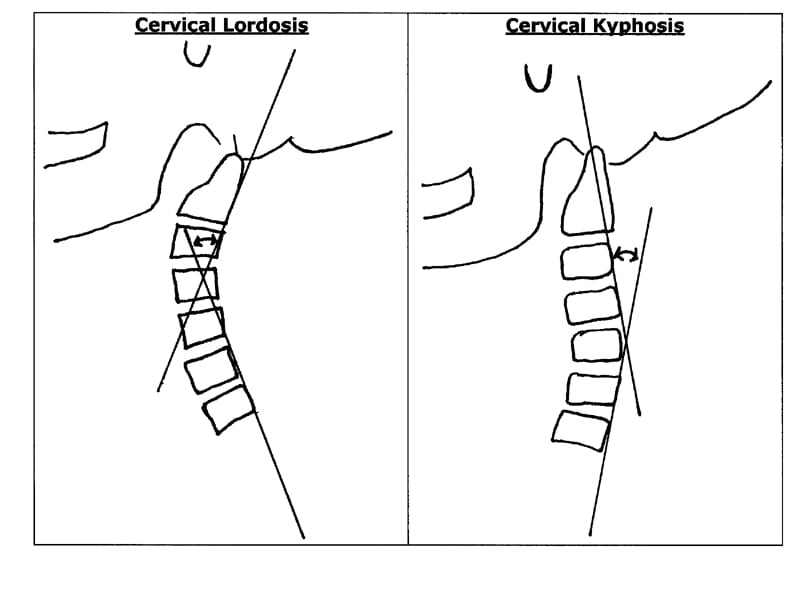
These authors evaluated 18 patients with cervical spine kyphotic deformity. The normal cervical spine has a gentle sloping, lordotic curve from C1 to C7. Cervical kyphosis refers to any degree of reversal of the normal cervical lordosis. Cervical alignment was assessed by lateral x-rays and the angle was measured on lateral x-rays by using tangential lines passing on posterior borders of adjacent vertebrae of apex kyphotic level.
This article emphasizes the adverseness of cervical spine kyphosis: accelerated spondylosis, spinal cord tethering, spinal cord ischemia, radiculopathy and myelopathy. The authors conclude that kyphotic angulation one level above the level of cervical disc disease “may be a factor in the development of cervical disc herniation and spondylosis, rather than its result.” They suggest that the kyphotic deformity be surgically corrected and stabilized if it measures more than 11 degrees.
•
In 2009, researchers from the Department of Orthopaedics and Rehabilitation Medicine, Fukui University, Japan, published a study in the Journal of Neurosurgery: Spine, titled (12):
Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment:
Outcome after Anterior or Posterior Decompression
This study looked at patients who had cervical kyphosis exceeding 10° on sagittal neutral lateral x-rays. The authors state:
“The kyphotic deformity associated with cervical spondylosis is the result of progressive subluxation of the apophyseal joints due to degenerative changes in the facet joints and discs.”
“We conclude that the [cervical spine] sagittal kyphotic deformity related to flexion mechanical stress may be a significant factor in the development of cervical spondylotic myelopathy.
•
These articles emphasize the adverseness of cervical spine kyphosis: accelerated spondylosis, spinal cord tethering and myelopathy. These studies indicate that cervical spine kyphosis is often a serious clinical finding, especially if greater than 10 degrees of angulation.
4
Is there any evidence that cervical spine kyphotic deformity can be improved or corrected with chiropractic management?
Chiropractic and x-rays were born in the same year, 1895. Some of the earliest spinal x-rays were performed by chiropractors. Chiropractors took x-rays to evaluate the biomechanics of the spine. For many decades, chiropractors have clinically noted that cervical spine kyphosis is associated with difficult and prolonged symptoms. Cervical kyphotic angulation displaces the center of gravity of the head anteriorly. This necessitates constant contraction of the posterior cervical musculature, resulting in fatigue and pain. Long-term follow-up studies of patients with cervical spine kyphosis document that these patients have acceleration of cervical spine spondylosis. More recent studies document that cervical kyphosis tethers the spinal cord, compromising spinal cord blood flow and resulting in myelopathy.
For decades, biomechanically based chiropractors have recognized the adverseness of cervical spine kyphosis. In the 1960s and 1970s, whiplash trauma expert Ruth Jackson, MD, (who also recognized the adverseness of cervical spine kyphosis) developed and researched the “Cervical Contour Pillow” in an effort to restore lordosis. The bulk of the chiropractic profession endorsed and adopted Dr. Jackson’s message and methodologies in cervical curve restoration.
In addition, chiropractic groups have researched other methods for treating cervical spine kyphosis and restoring cervical lordosis. These methods included certain adjusting methods, exercises, and traction protocols that involve cervical extension. These methods have proven to be successful (13, 14, 15, 16, 17, 18, 19, 20, 21).
SUMMARY
Repetitive microtraumatic events to the cervical spine, like “heading” soccer balls, initiates and accelerates cervical spine spondylosis.
A single macrotraumatic event to the cervical spine, like whiplash injury, initiates and accelerates cervical spine spondylosis.
The lateral cervical x-ray is the standard way to document the state of the cervical spine curvature.
Whiplash trauma to the cervical spine can cause cervical spine kyphotic deformity.
Post-traumatic cervical spine kyphosis is coupled with a poor prognosis for recovery. Consequently, cervical kyphosis is very important to document in whiplash-injured patients. Radiologist Lee Hadley, MD, states that the finding of cervical spine kyphosis should be considered to be a permanent injury.
Cervical spine kyphotic angulation has been shown to accelerate cervical spondylosis and spinal cord myelopathy.
Biomechanically oriented structural rehabilitation that includes postural training, specific spinal adjusting, exercises, and extension traction has been shown to improve and even reverse cervical spinal kyphotic deformity.
In patients with cervical spine kyphosis that cannot be conservatively corrected to less than 10 degrees should be surgically corrected and stabilized.
REFERENCES
1) Kartal A, Yldran B, Enköylü A, Korkusuz F; Soccer causes degenerative changes in the cervical spine; European Spine Journal, February 2004, 13(1):76-82.
2) Jackson R. The Positive Findings in Alleged Neck Injuries. American Journal of Orthopedics. 1964 Aug-Sep;6:178-87.
3) Hohl, M. The Cervical Spine; The Cervical Spine Research Society; Lippincott, 1989, p. 440.
4) Hamer AJ, Gargan MF, Bannister GC, Nelson RJ. Whiplash injury and surgically treated cervical disc disease. Injury. 1993 Sep;24(8):549-50.
5) Gargan MF, Bannister GC. The Comparative Effects of Whiplash Injuries. The Journal of Orthopaedic Medicine, 19(1), 1997, pp. 15-17.
6) Jackson R, The Cervical Syndrome, Thomas, 1978.
7) Hadley LA, Anatomico-Roentgenographic Studies of the Spine, fourth printing, Charles Thomas, 1979.
8) Griffiths HJ, Olson PN, Everson LI, Winemiller M. Hyperextension strain or “whiplash” injuries to the cervical spine; Skeletal Radiology. May 1995 ;24(4):263-6.
9) Giuliano V, Giuliano C, Pinto F, Scaglione M. The use of flexion and extension MR in the evaluation of cervical spine trauma: initial experience in 100 trauma patients compared with 100 normal subjects; Emergency Radiology (October 2002) 9: 249–253.
10) Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. European Spine Journal. August 2001;10(4):320-4.
11) Özer E, Yücesoy K, Yurtsever C; Seçil M. Kyphosis One Level Above the Cervical Disc Disease: Is the Kyphosis Cause or Effect? Journal of Spinal Disorders & Techniques; February 2007 – Volume 20 – Issue 1 – pp 14-19.
12) Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Kobayashi S, Baba H. Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment: Outcome after Anterior or Posterior Decompression. Journal of Neurosurgery: Spine; November 2009, Volume 11, pp. 521-528.
13) Leach RA. An evaluation of the effect of chiropractic manipulative therapy on hypolordosis of the cervical spine. J Manipulative Physiol Ther. 1983 Mar;6(1):17-23.
14) Harrison DD, Jackson BL, Troyanovich S, Robertson G, de George D, Barker WF. The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study.J Manipulative Physiol Ther. 1994 Sep;17(7):454-64.
15) Troyanovich SJ, Harrison DE, Harrison DD. Structural rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms. J Manipulative Physiol Ther. 1998 Jan;21(1):37-50.
16) Harrison DE, Harrison, DD, Haas JW. CBP Structural Rehabilitation of the Cervical Spine, 2002.
17) Harrison DE, Cailliet R, Harrison DD, Janik TJ, Holland B. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil. 2002 Apr;83(4):447-53.
18) Morningstar MW, Strauchman MN, Weeks DA. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study. J Chiropr Med. 2003 Spring;2(2):51-4.
19) Harrison DE, Harrison DD, Betz JJ, Janik TJ, Holland B, Colloca CJ, Haas JW. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003 Mar-Apr;26(3):139-51.
20) Ferrantelli JR, Harrison DE, Harrison DD, Stewart D. Conservative treatment of a patient with previously unresponsive whiplash-associated disorders using clinical biomechanics of posture rehabilitation methods. J Manipulative Physiol Ther. 2005 Mar-Apr;28(3):e1-8.
21) Oakley PA, Harrison DD, Harrison DE, Haas JW. Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc. 2005 Dec;49(4):270-96.