Athletically, at age 21, Dave was a rising star. He was tough, fit, tall, strong, and very fast. In addition, he was gifted with superior eye-hand coordination. As a life-long athlete, his favorite sport was football, and in football he was exceptional. Dave was the starting wide receiver on a local college football team.
Although his athletic scholarship covered his school expenses and tuition, off-season Dave worked in construction. This work was physically demanding, and Dave was easily able to meet those demands.
Dave’s attitude was so good both on and off the football field that he was a favorite of his coaches, teachers, construction job bosses, teammates, and coworkers. By all accounts, Dave had a bright future and would go far. His primary personal goal was to play pro football in the National Football League.
And then an accidental tragedy struck: a vehicle-to-vehicle collision. Dave was in a motor vehicle that was traveling about 25 miles per hour through an intersection that was controlled by a traffic light. The traffic light was green. While proceeding through the intersection, a second vehicle suddenly appeared “out of nowhere” directly in front of Dave’s vehicle, and there was a head-on collision. The police report estimated the speed of the other vehicle to also be about 25 miles per hour. The “other” driver was cited for causing the accident.
Both vehicles were of approximately the same size (mass). The damage to both vehicles was moderate, but bad enough that both had to be towed away from the accident scene. Yet, the air bags did not deploy.
Four football players occupied Dave’s vehicle (Dave and 3 of his teammates). Dave was not the driver; rather he was the front seat passenger. Only Dave was wearing his seat belt; the other 3 young men were unbelted.
The collision caused an abrupt halt to the forward motion of Dave’s vehicle. Yet, according to Newton’s Law of Inertia, the 4 young men in the vehicle continued to move forward at about 25 miles per hour. Often this mechanism is referred to as the occupants being “thrown forward.” In reality, they are not “thrown forward.” Rather, their bodies continue to move forward at the vehicle’s speed of 25 miles per hour, thus colliding with vehicle structures that are in front (“forward”) of them. The 2 unbelted back seat passengers collided with the back of the front seats. The unbelted driver collided with the steering wheel, but not with the dashboard or windshield.
Dave (seating in the front passenger seat), did not collide with the interior of the vehicle because he was belted. Specifically, Dave was wearing the standard lap-shoulder belt combination. The seat belt Dave was using possessed a standard locking mechanism; when subjected to a sudden jerk, it locked. The quick inertial jerk on the belt caused by the forward inertial movement of Dave body initiated the jerk-locking mechanism, effectively stopping Dave’s forward inertial movement.
However, there are a few problems with the standard lap-shoulder belt combination. Specifically, in this case, the shoulder portion of the belt cut across Dave’s right clavicle, effectively stopping the forward motion of his right shoulder. This design did not stop the forward motion of Dave’s left shoulder or the forward motion of his head. However, the lap portion of the belt quickly locked, stopping the forward motion of Dave’s lower trunk.
As irony would have it, Dave’s 3 unbelted teammates were not injured. Although they were all “thrown forward” by the impact and collided with aspects of the vehicle’s interior, none of them ever developed any musculoskeletal complaints or consulted any health care providers for signs or symptoms caused by this collision.
During motor vehicle collisions, serious and fatal injuries often occur when occupants experience:
1) Crushing injuries
2) Inertial injuries that involve hitting the steering wheel, windshield or dashboard
3) Inertial injuries where occupants are thrown from the vehicle
Over the decades, motor vehicle safety engineers have added safety devices to automobiles to reduce these categories of serious injury and/or death risk. The primary focus has been on seat belts (initially) and air bags (more recently).
There is no doubt that current generation air bags save lives when they deploy. They do so primarily as a consequence of preventing the front seat driver and passenger from hitting the steering wheel, dashboard, and windshield. However, the initiation of the air bag inflation sequence requires a certain threshold. This threshold is determined by the degree of the front of the vehicle crumpling. If this threshold is not reached, the air bag inflation sequence will not be initiated and the air bag will not deploy. The collision Dave and friends experienced did not meet the air bag inflation threshold and the air bags did not deploy.
The primary purpose for vehicle seat belts is to prevent occupant ejections as a consequence of inertially based forces. The experience of being thrown from a vehicle during a collision is often fatal or associated with life-long impairments. Seat belts are excellent at preventing vehicle occupants from being thrown out of the vehicle during a collision (ejected). Consequently, there is no doubt, seat belts save lives.
However, more than half a century ago, it was noted that seat belts themselves could cause injuries. There are primarily two injuries associated with this:
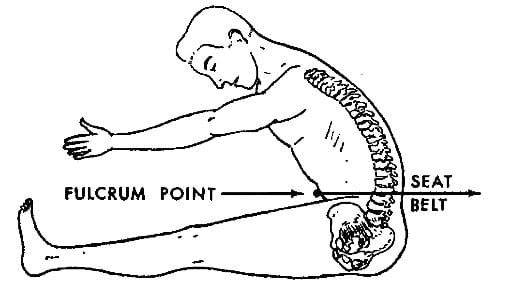
1) The lap belt alone does not stop the forward inertial motion of the trunk above the belt or the pelvis and legs below the belt. Lap belts alone concentrate the inertial forces to the small (a few inches) cross sectional dimension of the belt. This allows the lap belt to function as a fulcrum of a first class lever mechanical system (a teeter totter). When the portions of the body above and below the belt continue in forward motion, the stresses at the fulcrum (the belt) are magnified, resulting in increased injury to the tissues behind the lap belt. These tissues include abdominal viscera (including the mesenteric arteries), the spine and its associated soft tissues (Thompson, 2001; Hall, 2001).
2) The addition of a (unilateral) shoulder harness will reduce the forward inertial motion of the trunk that lies above the lap portion of the belt. This is largely desirable, but not without its own complications. The primary benefit is a significant reduction of lap belt fulcrum injuries. The complications of the (unilateral) shoulder harness include:
A) The shoulder harness does not stop the forward inertial motion of the head. Since the addition of the shoulder harness reduces the forward motion of the trunk but not that of the head, there is an increase in the inertial stresses the cervical spine experiences. This is not good for the neck. There is clear documentation that the incidence of neck sprains has increased since the use of lap/shoulder belt combination became compulsory (Rutherford, 1985).
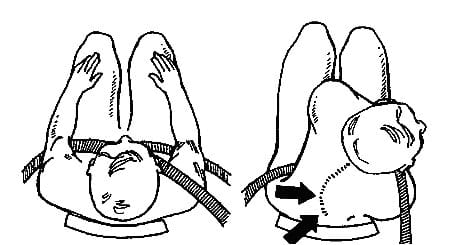
B) Since the shoulder harness only restrains one shoulder, the forward inertial motion of the other shoulder introduces a rotational or twisting mechanism to the torso (Anrig, 1998). The implications for this are discussed below.
(From Anrig)
C) The shoulder harness increases injury to the chest wall, sternum and clavicle (Greingor, 2006).
D) The shoulder harness increases injury to the breast (DiPiro, 1995; Majeski, 2007; Paddle, 2010).
The 3 occupants in Dave’s vehicle who were not restrained with seat belts were not ejected from the vehicle in this collision. Although their bodies collided with various parts of the vehicle’s interior, the impact forces were distributed over large enough areas of their bodies that no specific body part was overtly traumatized. In other words, the forces were distributed over a large surface area. Again, none of these 3 young men developed any symptoms or signs of injury from this collision.
Dave however was less fortunate. Dave was injured. The basis for Dave’s injuries are as follows:
1) The collision caught Dave completely by surprise. Consequently, he was unable to brace against the forces that were imparted into his body. In such a scenario, muscle injury is reduced but articular injury (intervertebral disc and facet capsule, etc.) are increased. It is established that being “caught by surprise” during a motor vehicle collision is coupled with greater injury, more symptoms, and a poorer recovery prognosis (Sturzenegger, 1994).
2) Dave was the front seat passenger, wearing a lap seat belt and a shoulder harness that cut across his right shoulder. As discussed above, this shoulder harness restrained the forward inertial movement of his right shoulder, but not his left shoulder. As discussed above, as Dave’s left shoulder moved forward in relation to his right shoulder, his trunk/torso twisted (rotated) to his right.
(From Anrig)
3) The forward, twisting motion of Dave’s left shoulder caused additional flexion of his trunk/torso about the lap portion of his seat belt.
In summary, during this collision and because of the lap belt and shoulder harness restraints, Dave sustained a flexion/rotation injury to his lumbar spine. Trunk/torso flexion and rotation in combination is a classic mechanism to injure and herniate a lumbar intervertebral disc. Ironically and without question, if Dave had been not restrained, as was the case with his 3 companions, he would not have sustained this low back disc herniation injury.
At the accident scene, Dave knew he was injured. For the first time in his life his back hurt and his legs did not feel right. But unsurprisingly, he did not immediately go to any health care provider, assuming that he would be fine in a day or two. However, after a few days of rest, his condition was not improving, and even appeared to be getting worse. The over-the-counter nonsteroidal anti-inflammatory drugs he was taking were not helping. Dave’s low back hurt, and it was very stiff. In addition, the pain in his legs went all the way down to his feet.
Dave presented at his HMO for an evaluation 4 days after being injured. Although his low back remained very painful and his legs ached all the way down to his feet, there was no indication of altered function of bowel of bladder function. His examination was unremarkable with the exception of spasm and reduced motion of this lumbar spine. X-rays of his lumbar spine were taken. There were no signs of fracture, dislocation, instability, or degenerative changes. Dave was diagnosed with a sprained back. He was encouraged to rest and to continue taking his pain medicines.
A week later (11 days after being injured), Dave was still in bad shape. He was not getting better, and he was discouraged. His three companions who were in the vehicle with him during the collision seemed to be perfectly fine with no symptoms at all. Dave decided to see a chiropractor to see if chiropractic could help him.
Dave presented himself to my office for examination and treatment on the 11th day following the collision and injury. History indicated that Dave felt he was getting worse, not better. Although his back was quite painful and stiff, his legs ached and they felt weak and clumsy.
It is our standard inquiry to ask about bowel, bladder, and sexual function. Dave replied that he had no opportunity or desire for sexual activity (he hurt too much), that his bowel movements were rare since injury (again, he blamed it on the pain it caused his back), but he did note that he was having a lot of trouble starting the stream for urination. He also noted that when he urinated, not much urine was produced, as if his bladder was not fully emptying. Dave noted that his bladder problems seemed to be getting worse over the last week or so.
Dave’s cervical spine was asymptomatic. Even so, I examined it, performing range of motion, compression tests, stretch tests, upper extremity deep tendon reflexes, superficial sensation and myotomal strength. The results for these procedures were unremarkable, essentially negative.
As a consequence of Dave’s lower back and lower extremity complaints, I thoroughly examined his back and legs. My finding include:
• Superficial sensations on his legs were normal.
• Patellar and Achilles deep tendon reflexes were quite suppressed bilaterally; in fact, I was unable to elicit them. I have seen this on other patients, and it can just be a normal variant, having no clinical relevance. However, it could also be an indication of a more serious low back nerve compression syndrome. If so, the syndrome would have to be affecting more than one nerve root (the Patellar reflex is controlled by the L2-3-4 roots; the Achilles reflex is controlled by the S1 root), and it would have to be bilateral.
• All of the myotomes tested in Dave’s legs were weak bilaterally, especially for a person so young and with a recent history of superior athletic ability. The muscles tested included the iliopsoas (L2-3-4), the quadriceps (L2-3-4), the tibialis anterior (L4), the extensor hallucis longus (L5), and the gluteus maximus (S1). These findings are inconsistent with a singe level of nerve root compressive neuropathology. Rather, they suggest that Dave has a compressive syndrome affecting multiple levels bilaterally.
• The Valsalva test was positive for a worsening of both low back and leg pain bilaterally. The Valsalva test is performed by attempted exhalation against a closed airway, usually done by closing one’s mouth and pinching one’s nose shut. Neuro-orthopedically it indicates that the patient has a space occupying lesion in the painful region of the spinal canal. The most classic space occupying lesion is a herination of the intervertebral disc into the central neural canal.
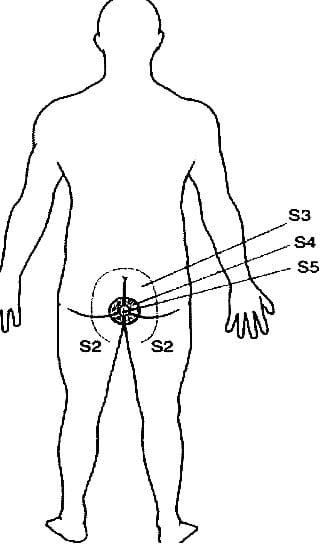
• I routinely assess superficial sensation in the lower extremities. In Dave’s case, they were unremarkable, normal. However, lower extremity dermatomes do not include S2-3-4-5. These sacral nerve roots innervate the perineum, which is the skin around the anus and buttocks. I do not routinely assess these sacral dermatomes because of the sensitivity of the anatomical parts necessary (around the anus), but in Dave’s case I felt it important to do so. Dave’s sacral dermatomes displayed a significant hypoesthesia, a reduced ability to feel the sensations of pin prick and light touch. This is known as “saddle anesthesia.”
This is a very important finding because in adults, the sacrum is fused into a single bony mass, the sacrum. Therefore, the only way multiple sacral nerve roots could be dysfunctional is for there to be a compression of the sacral roots at the cauda equina of the lumbar central neural canal. The most probable cause of the compression is a midline herniation of a lumbar intervertebral disc.
In Dave’s case, everything seemed to add up to a single conclusion:
• All symptoms and signs began with a single traumatic event 11 days prior.
• The mechanism of injury included a forward inertial propulsion around a fulcrum lap belt with a degree of rotation caused by the shoulder harness. A flexion/rotation event is a classic mechanism to injure the intervertebral disc and cause a posterior herniation. The fulcrum lap belt injury is proven to increase injury to the lumbar spine and discs.
• Dave’s primary symptoms include back pain, leg pain to the feet, and difficulty initiating the urinary stream.
• Dave’s examination includes a positive Valsalva test, consistent with a posterior lumbar disc intervertebral disc herniation into the lumbar spine central canal.
• Lower extremity myotomal weakness and depressed deep tendon reflexes are consistent with compressive neuropathology to multiple lumbar roots, bilaterally.
• Dave has saddle anesthesia.
Dave is suffering from a traumatically induced cauda equina syndrome.
Cauda Equina syndrome is not a chiropractic case; they should not be managed by a chiropractor. In fact, they are medical emergencies. When a cauda equina syndrome is suspected, the patient should be referred out as a medical emergency. Timing is critical in the management of cauda equina syndrome; a delay in decompression can result in permanent problems in the legs, sexual function, bladder function, and/or bowel function. A 2008 article in the Journal of the American Academy of Orthopedic Surgeons (Spector) makes the following points:
Cauda equina syndrome is a relatively uncommon condition typically associated with a large, space-occupying lesion within the canal of the lumbosacral spine.
The syndrome is characterized by varying patterns of low back pain, sciatica, lower extremity sensorimotor loss, and bowel and bladder dysfunction.
The pathophysiology remains unclear but may be related to damage to the nerve roots composing the cauda equina from direct mechanical compression and venous congestion or ischemia.
Early diagnosis is often challenging because the initial signs and symptoms frequently are subtle.
Classically, the full-blown syndrome includes urinary retention, saddle anesthesia of the perineum, bilateral lower extremity pain, numbness, and weakness.
Decreased rectal tone may be a relatively late finding.
A high index of suspicion is necessary in the spine patient with back and/or leg pain refractory to analgesia, especially in the setting of urinary retention.
Regardless of the setting, when cauda equina syndrome is diagnosed, the treatment is urgent surgical decompression of the spinal canal.
A few hours later, on my referral, an MRI was performed on Dave’s lumbar spine. The results showed a large posterior midline herination of the L5 intervertebral disc into the lumbar central neural canal, compressing the cauda equina. My diagnosis was essentially confirmed.
Dave underwent decompressive surgery the following day. The neurosurgeon felt Dave would have an instability as a consequence of the discectomy and proceeded to stabilize Dave’s L5-S1 articulation with an interbody fusion.
Myself and our office performed Dave’s post surgical rehabilitation. Our management included graded range of motion and resistive effort exercises, myotherapy, postural corrections, management of articular dysfunctions, anti-inflammatory diet and nutrition, and low level laser therapy.
The good news is that Dave enjoyed a good clinical recovery. His bowel and bladder function returned to normal and he suffered from no functional residuals. His leg pains also resolved. He does retain residual low back stiffness and some lower back pain, especially at times of increased use or stress.
The bad news is that Dave was no longer able to participate in college football, and any chance of professional football play ended. Also, he was no longer able to work construction.
Dave’s injury case went to a jury trial. Dave’s neurosurgeon testified as to the necessity of the surgical decompression and subsequent stabilization. He also testified that the need for the surgery was 100% as the result of the injuries sustained in the automobile accident.
I also testified in Dave’s trial. My testimony centered around the necessity of the rehabilitation program we did on Dave, as well as quantifying his permanent restriction in work and leisure activities. I testified that 100% of our rehabilitation program and his permanent residuals were attributable to the injuries sustained in the accident.
As a consequence of my extensive writing and teaching on the topic of whiplash biomechanics, I qualified as an expert to explain the mechanism of Dave’s injuries during this collision. This was important because it was the position of the defense that Dave could not have been injured in this accident as none of the other three young men sustained any injuries at all. Apparently the jury liked my explanation, as it is logical and supported by the literature. Had I not qualified to testify on mechanism, I believe the outcome would have been much different for Dave. Dave’s monetary award was in the six figures.
Dr. Dan Murphy
REFERENCES
Thompson NS, Date R, Charlwood AP, Adair IV, Clements WD.
International Journal of Clinical Practice. Seat-belt syndrome revisited; October 2001; Vol. 55; No. 8; pp. 573-5.
Hall CE, Norton SA, Dixon AR. Complete small bowel transection following lap-belt injury; Injury October 2001; Vol. 32; No. 8; pp. 640-1.
Rutherford WH; The Medical Effects of Seat-Belt Legislation in the United Kingdom: a critical review of the findings; Archives of Emergency Medicine, 1985, 2, 221-223.
Anrig C, Plaugher G; Pediatric Chiropractic, Williams & Wilkins, 1998.
Greingor JL, Lazarus S; Chest and abdominal injuries caused by seat belt wearing; Southern Medical Journal; May 2006;Vol. 99; No. 5; pp. 534-5.
DiPiro PJ, Meyer JE, Frenna TH, Denison CM. Seat belt injuries of the breast: findings on mammography and sonography. American Journal of Roentgenology; Feb 1995;Vol. 164; No. 2; pp. 317-20.
Majeski J. Shoulder restraint injury of the female breast; International Surgery; Mar-Apr 2007; Vol. 92; No. 2; pp. 99-102.
Paddle AM, Morrison WA; Seat belt injury to the female breast: review and discussion of its surgical management. ANZ Journal of Surgery. January/February2010; Vol. 80; No. 1-2; pp. 71-4.
Sturzenegger M, DiStefano G, Radanov BP, Schnidrig A; Presenting symptoms and signs after whiplash injury: the influence of accident mechanisms; Neurology; April 1994; Vol. 44; No. 4; pp. 688-93.
Spector LR, Madigan L, Rhyne A, Darden B 2nd, Kim D; Cauda equina syndrome; Journal of the American Academy of Orthopedic Surgery; August 2008; Vol. 16; No. 8; pp. 471-9.