John, a 55-year old male, was an urban cowboy. John did not own any property (other than his tract home), cattle, or horses. As the floor foreman of a large manufacturer, his job required him to be on his feet most of the day with a moderate requirement for physical lifting and equipment operation. John was healthy, strong, and very active in both his professional life and his leisure activities. His favorite recreational activity was dancing nearly every night, primarily country-western line dancing.
John’s attire was usually western, including boots, jeans, button-down shirt, cowboy hat, and a pair of sunglasses. John drove a small 4-wheel drive pick-up truck with an extended cab.
On a busy Friday afternoon, John was driving home from work when the freeway traffic suddenly stopped, and John successfully and safely stopped. However, the large SUV behind him, driven by a distracted young female, did not successfully stop, and slammed into the rear of John’s truck.
The noise was deafening. The impact was great enough to propel John’s vehicle into the vehicle in front of him.
John was wearing a shoulder-lap type of seat belt. Although the front of his truck sustained substantial damage from slamming into the vehicle in front of him, his air bag did not deploy. The collision had caught John completely by surprise. Importantly, John was no longer wearing his cowboy hat or his sunglasses; both were found behind his seat, in the extended cab portion of his truck. The fact that the hat and sunglasses, having their own inertia, landed in the back of his truck, suggests that for a brief moment, John’s head, hat, and glasses were in the back portion of his truck. When John’s truck was abruptly halted from colliding with the vehicle in front of his, his head was inertially quickly thrown forward, leaving his hat and glasses behind.
Although dazed and confused, John immediately perceived that he was injured, but he was not sure how badly. His vehicle was destroyed and was not drivable. All adjacent traffic had halted, allowing John to carefully push open his door and exit his truck. Upon standing, he felt unsteady, and his legs did not feel right. As he took a few steps he thought he would fall over, and to compensate he broadened his stance and gate, and shortened his stride. John’s neck also hurt, but he was more concerned about the strange sensations he was having in his legs and his inability to walk correctly.
In about 20 minutes, an ambulance appeared at the accident scene. The paresthesias and motor difficulties in John’s lower extremities concerned the ambulance crew. The crew quickly applied an immobilization device to John’s thoraco-lumbar spine, and he was transported to a local hospital.
The hospital emergency personnel were primarily concerned with trauma induced neurological compromise, hence the on scene immobilization. Because John’s major symptoms were associated with his lower extremities, the immediate urgency was to rule out fracture/dislocation of the lumbar or lower thoracic spine. Radiographs were therefore exposed. Findings were negative.
Negative radiographs with ongoing symptoms prompted additional diagnostic imaging. An MRI of the entire lumbar spine and lower thoracic spine was exposed. Once again, findings were negative. There were no signs of fracture, dislocation, edema, hematoma, or any other type of space occupying pathology. The lower spinal cord, the cauda equina, the lumbar spinal roots and the sacral roots all appeared to be normal without any pathology.
John’s walking intolerance and gait abnormalities remained unexplained. There simply were not any positive examination findings to account for his maladies. Perplexed, his health care providers recommended physical therapy to his lower extremities and gait rehabilitation.
John was quite distressed. His primary leisure enjoyment was dancing, an activity that he was no longer capable of performing. He dutifully attended his physical therapy appointments for the next three months. John had physical therapy three times per week for the next three months. His therapy consisted primarily of gait training as well as lower extremity muscle stretching and strengthening exercises. After these three months, there was no improvement.
John was now desperate and frustrated; and so was his wife (Phyllis). Phyllis happened to be John’s dance partner; when John could not dance, Phyllis could not dance. Their social life had regressed to near zero, and their social contacts were greatly compromised. Phyllis insisted that John do something different. A friend of hers knew and recommended that she take John to her (the friend’s) chiropractor.
•••••
Different parts of the human body have different inertial masses. The mechanism of injury from a rear-end motor vehicle collision, is, as a rule, an inertial injury. This means the injury does not occur as a consequence of direct contact of vehicle parts to the patient’s body; rather, injury occurs as a consequence of different inertial masses moving independently from one another.
The primary inertial stresses experienced by those involved in a rear-end motor vehicle collision is between the head and the trunk. Technically, when a vehicle is struck from behind, the entire vehicle is propelled forward, including its frame, seats, and the trunk of those sitting in those seats. However, the head, having a different inertia than the trunk, will follow Newton’s Law of Inertia (1), and remain stationary. Essentially, the trunk is moved under the head as the head remains still. This puts an inertial load onto the structure responsible for balancing the two large inertial masses (the head and trunk) to each other, the cervical spine (neck). The neck actually never hits anything; it sustains an inertial injury.
Although there are a number of variables that must be accounted for in any particular collision, in general, the magnitude of the inertial injury to the neck is linked to the magnitude of the acceleration achieved by the struck vehicle. This is why authoritative reference texts pertaining to whiplash collisions are subtitled the “Cervical Acceleration Deceleration Syndrome” or CAD (2). Importantly, it is understood that large vehicle accelerations and subsequent cervical spine inertial injuries can occur when the struck vehicle sustains little or even no damage.
In John’s case above, there was not one, but two distinct inertial injury mechanisms. The first was the rear-end collision, delivering the inertial injuries as a consequence of acceleration. The second was a deceleration injury.
After being struck from the rear and accelerating forward, John’s vehicle struck the vehicle in front of him and his vehicle came to a sudden halt. However, in accordance with the Law of Inertia, John’s body and head continued to move forward and, in the absence of safety devices, his body and head would slam into his vehicle’s dashboard, steering wheel, and windshield. Fortunately, as noted above, John was wearing his lap-shoulder restraint belt, which soon engaged, stopping the forward propulsion of his body short of the steering wheel and dashboard. Unfortunately, the lap-shoulder restraint does not stop the inertial movement of the head. Consequently, the head, being in motion will continue in motion until encountering some resistance. Usually, this resistance is the chin hitting the chest, and thus adding cervical spine deceleration inertial injuries to the acceleration cervical injuries he sustained just moments before.
Historically, most vehicle collision fatalities occurred when the subject was thrown from the vehicle, a common occurrence in head-on collisions. As an example, if a vehicle traveling at 50 miles per hour collides with an immoveable object, such as a tree or a wall, the vehicle may abruptly stop, but the person’s body in that vehicle would continue to travel forward at 50 miles per hour, greatly increasing the risk of being thrown from the vehicle.
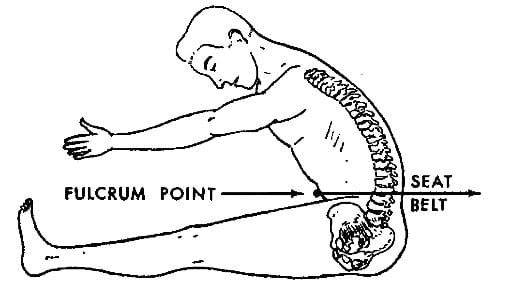
To reduce the risk of such ejections, lap belts were installed in vehicles, and it eventually became mandatory to use them. Lap belts greatly reduced ejections and therefore fatalities, but by 1948 it was documented that during the forward phase of a collision, the lap belt functioned as a fulcrum, concentrating an inordinate amount of forces to the region of the belt placement (3). The results were again, fewer ejections and fatalities, but an increase in devastating thoraco-lumbar spinal injuries and abdominal visceral injuries.
To remedy these thoraco-lumbar spinal injuries and abdominal visceral injuries, the lap-shoulder restraint was developed. The inclusion of the shoulder harness significantly reduced thoraco-lumbar spinal injuries and abdominal visceral injuries, but another problem was documented: the shoulder harness stopped the forward motion of the trunk, but the head continued in forward motion. This subjected the cervical spine to tremendous deceleration inertial stress with devastating cervical spine flexion injuries.
The solution to the problem of shoulder restraint cervical spine inertial injuries depended upon the arrival of new technology: a sensor in the hood of the vehicle that, when sufficiently mechanically stressed, would initiate inflation of an airbag. This airbag, a gaseous filled cushion, would stop the forward movement of the head, reducing the magnitude of cervical spine inertial injuries. Unfortunately for John, for reasons unexplained, his vehicle’s air bag did not deploy, even though the front of his vehicle was significantly crumbled.
•••••
Although John’s primary complaints were in his lower extremities, mechanistic understanding and history indicate that the primary inertial forces (and therefore probable injuries) were to his cervical spine. It is well established that the primary injury to the cervical spine during a motor vehicle collision is to the facet joint capsules. It is also documented that the second most prevalent injury to the cervical spine is to the intervertebral disc. It is established that inertial cervical spine injuries sustained during motor vehicle collisions can herniate the cervical disc, resulting in radiculopathy and/or myelopathy.
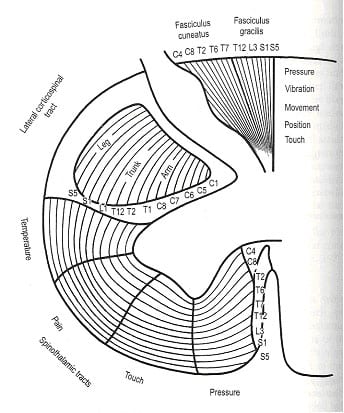
Viewing an axial cut through the cervical spinal cord shows that the motor and sensory nerves of the cord are arranged in layers. Importantly, the outer nerve fibers, the ones that would be most vulnerable to compressive myelopathy from a disc herniation, innervate the lower extremities.
From Gray’s Anatomy, 39th edition, 2005, p. 318
There is no doubt that a cervical spine intervertebral disc herniation can result in motor and sensory complaints in the lower extremities, and this can occur in the absence of significant neck complaints (4).
In compressive neuropathology, large diameter nerve fibers are more vulnerable than are small diameter nerve fibers. Importantly, pain afferent nerve fibers are small diameter, and consequently less vulnerable to compressive neuropathology. In contrast, large diameter fibers are associated with proprioception, positional sense, gate stability, and motor control. These fibers and functions are most vulnerable to compressive neuropathology.
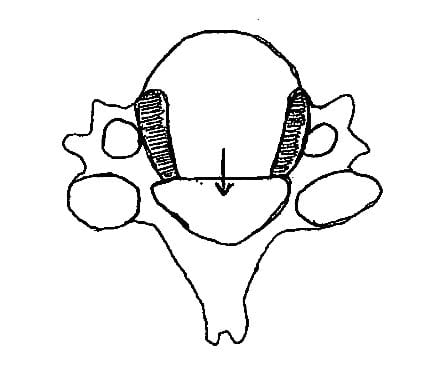
Posterior midline cervical disc herniations occur more commonly than do posterior-lateral or lateral herniations. This is attributed to the presence of the uncinate processes (joints of von Luschka):
Uncinate Processes
The uncinate processes resist lateral and postero-lateral disc herniations, but allow the disc to herniate midline posteriorly.
These joints form a wall or barrier to lateral and/or posterior-lateral cervical disc herniations. The path of least resistance is posterior. Such a midline herniation would spare the cervical nerve roots and thus there would be no classical symptoms or signs of cervical spine radiculopathy. However, should the midline posterior disc herniation be large enough, it could mechanically compromise the spinal cord (myelopathy). The associated symptoms and signs would be long tract signs affecting the lower extremities. Because the nature of the lesion would be characterized as compressive myelopathy, large diameter nerve function would be most influenced (proprioception, positional sense, gate stability, and motor control).
The posterior midline cervical disc herniation would effectively narrow the sagittal diameter size of the cervical spinal canal. The technical diagnosis for such an occurrence is “central canal stenosis.” The cervical central canal is reduced in extension (further compromising the spinal cord) and enlarged in flexion. Consequently, extension positions will aggravate the symptoms and signs associated with central canal stenosis and its associated myelopathy; flexion positions will improve the associated symptoms and signs (5).
•••••
………. Within a few days, and just over three months after being injured, John reluctantly presented himself as a new patient in my office. His clinical symptoms and status were unchanged: his legs felt “funny” tired and heavy; he could not walk normally, his stance being wide and his stride being short and choppy; he felt unsteady, as if he might fall down because of his dysfunctional legs. He was anxious, irritable, and skeptical.
Upright lumbar, thoracic, and cervical biomechanical x-rays were exposed. There was no sign of any pathology such as fracture, dislocation, or degenerative disease. However, the lateral cervical x-ray showed a sharp reversal of the normal lordotic curve; the kyphotic angle measured 10 degrees, its apex at the C5-C6 interspace.
John’s initial examination showed normal deep tendon reflexes, myotomal strength, and superficial sensations on both his lower and upper extremities. These findings seemed inconsistent with his lower extremity complaints. Lumbar and thoracic ranges of motion were slightly reduced but non-painful. Lumbar spine compression tests did not aggravate any of his complaints. The straight-leg-raising tests were completed to an arc of 45 degrees and produced no additional symptoms.
John’s cervical ranges of motion were significantly reduced. He added that his neck was quite stiff and sore. The cervical spine axial compression test was uncomfortable and it produced an uncomfortable sensation between his shoulder blades.
John’s plantar reflex (Babinski’s sign) was normal (toe down). Vibration sense was intact on his fingers and toes. He was flawless in knowing the position of his toes when they were purposefully moved up or down (positional sense).
Overall, John was a challenging case. History, presentation, education, experience, and intuition all told me his problem was in his cervical spine. Although his main complaints were his legs and gait, most of his abnormal examination findings were in his cervical spine. This included a sharp kyphotic angulation. It appeared to me that stressing his neck may change some of his examination findings.
I gently placed John supine with his head over the end of the examination table. In other words, his head and neck were in an extension position. I left John in this position for 30 seconds. After 30 seconds, while his head/neck were still extended, I redid the plantar reflex (Babinski’s test). He had an immediate and significant up-going toe, an abnormal finding. The up-going toe during the plantar reflex is indicative of a problem with the spinal cord, or possible brain, what is classically known as an “upper motor neuron lesion.” While remaining in cervical extension, retesting of both his patellar and Achilles’ deep tendon reflexes found them to be hyper-reactive while in that position. This is also abnormal and indicative of an upper motor neuron lesion.
While remaining in cervical extension, John also lost the ability to perceive vibration in his toes, and he lost the ability to perceive the up-down position of his toes. Both of these functions are associated with large diameter neurons. This indicates that large diameter neuron function was compromised while John was in cervical spine extension.
My working diagnosis was that John was suffering from a traumatic midline posterior disc herniation that was causing cervical spine central canal stenosis and compressive myelopathy, resulting in long tract signs (motor and sensory) to his lower extremities. My working diagnosis is based upon these factors:
• Mechanism of injury was both a rear-end collision followed moments later by a head-on collision. Both collisions imparted significant inertial loads to the cervical spine. Such collisions and inertial loading are known to cause disc herniations.
• There were no signs of upper extremity motor or sensory radiculopathy.
• There were no signs of lower extremity motor or sensory radiculopathy.
• Three months of treatment of the lower extremities did not result in improvement. There had been no investigations or treatment given to the cervical spine.
• Examination found the neck to be significantly stiff, and John complained that it felt stiff and sore.
• Cervical spine compression caused interscapular pain (pain between the shoulder blades). It has been known since 1959 that cervical disc disease often causes interscapular pain (6).
• X-rays showed a sharp reversal of cervical kyphosis. This is consistent with discogenic central canal stenosis and cervical cord myelopathy (7).
• The outer nerve fibers of the spinal cord arise from (afferents) and innervate (motor) the lower extremities.
• Central canal stenosis and its attendant myelopathy are aggravated in extension (5). Extension worsens compressive myelopathy because the central canal becomes smaller in extension.
• Compressive neuropathies (including myelopathy) primarily affect the function of the large diameter neurons, including the perception of the modalities of positional and vibratory sense.
• It is documented that cervical spine stenosis with myelopathy causes a walking intolerance, such as John’s (8).
I informed John that he needed an MRI. He quickly snapped that he already had one and it was normal. I politely said he needed an MRI of his neck. He quickly questioned the reason, reminding me that it was his legs that were dysfunctional. I replied “exactly.” I showed John my rationale, convincing him to follow my recommendations.
The MRI of John’s cervical spine showed that 50% of the central neural canal was occupied by a midline posterior disc herniation, pressing on the anterior spinal cord (myelopathy), as suspected. Because of the large displacement, I referred John to a neurosurgeon for a surgical consult. The neurosurgeon felt that John should have a surgical decompression. John asked me for a second surgical opinion, so I next referred him to an orthopedic surgeon who specialized in spinal surgeries. The orthopedic surgeon also suggested a surgical decompression.
John was hesitant to do surgery, especially since no one had yet tried conservative management of his neck; if fact, so far no one had treated his neck at all. John asked me if I would be willing to treat his neck for a month or so, hoping that he might improve and avoid surgery. I agreed. I used the basic protocols outlined by Joel and Jeffery Saal in the journal Spine in 1996 (9). This protocol included a combination of mobilization, strengthening exercises, and most importantly, daily cervical spine traction. I also dealt with his postural alignment and I put him on an anti-inflammatory diet, including 3 grams per day of omega-3 fatty acids (fish oil).
John’s disc herniation was very large, more than the 4 mm threshold Saal and Saal describe in their article (9). Yet, the combination of the program of care I outlined for him worked quite well. He slowly began to improve. Both his neck and lower extremity symptoms began to improve. I treated John in the clinic 32 times over a period of 18 weeks (4.5 months). He dutifully did his home traction, four times per day, 10-15 minutes each time.
John was able to avoid surgery. He is back dancing, with his wife, Phyllis.
Dan Murphy, D.C.
REFERENCES
1) Newton I; Mathematical Principles of Natural Philosophy; 1687.
2) Foreman SM, Croft AC; Whiplash Injuries; The Cervical Acceleration / Deceleration Syndrome; Williams & Wilkins; 1988.
3) Chance GQ; Note on a Type of Flexion Fracture of the Spine; British Journal of Radiology; 1948; Volume 21; Number 249; pp. 452-453.
4) Kabat H, Low Back and Leg Pain From Herniated Cervical Disc, Warren H Green, 1980.
5) Bland J, Disorders of the Cervical Spine, WB Saunders Company, 1987.
6) Cloward RB; Cervical Diskography, A Contribution to the Etiology and Mechanism of Neck, Shoulder and Arm Pain; Annals of Surgery; December 1959; Vol. 150, No. 6; pp. 1052-1064.
7) Kenzo Uchida, Hideaki Nakajima, Ryuichiro Sato, Takafum i Yayama, Erisa S. Mwaka, Shigeru Kobayashi, Hisatoshi Baba; Cervical Spondylotic Myelopathy Associated with Kyphosis or Sagittal Sigmoid Alignment; Journal of Neurosurgery: Spine; November 2009, Volume 11, pp. 521-528.
8) Kikuchi S, Watanabe E, Hasue M, Spinal intermittent claudication due to cervical and thoracic degenerative spine disease, Spine, February 1, 1996, 21(3):313-8.
9) Saal, Joel S. MD; Saal, Jeffrey A. MD; Yurth, Elizabeth F. MD; Nonoperative Management of Herniated Cervical Intervertebral Disc With Radiculopathy; Spine; Volume 21(16) August 15, 1996, pp 1877-1883.