What is a Whiplash Injury?
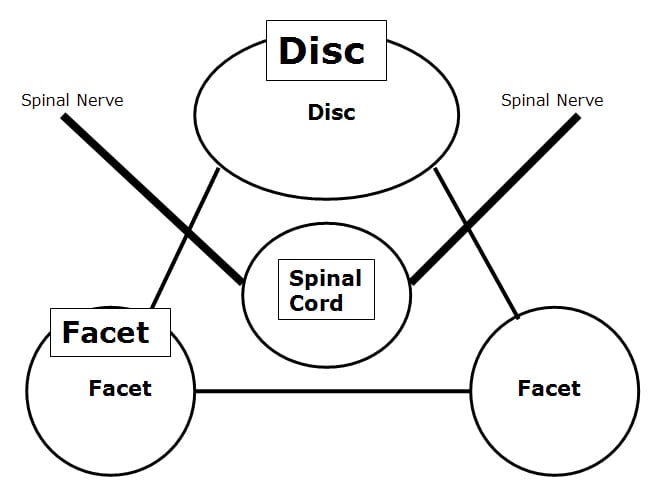
Whiplash injuries have been extensively studied and researched. There are literally thousands of medical and scientific studies, and hundreds of books describing every aspect of whiplash injury. It has been firmly established for nearly two decades that the primary whiplash injury is an inertial injury to the soft tissues (ligaments and muscles) of the facet joints and disc joint of the cervical spine.
Sir Isaac Newton was an English physicist, mathematician, astronomer, natural philosopher, and theologian. Newton spent his career at the University of Cambridge, England. In 1687, at the age of 43, Newton published the book Principia Mathematic, which is among the most influential books in the history of science. In Principia Mathematic, Newton describes the three Laws of Motion. It is Newton’s Laws of Motion that explain contemporary whiplash trauma and subsequent injury. The most important Law is his first, often referred to as the Law of Inertia. Simply stated in the context of whiplash injury, things at rest tend to remain at rest and to resist change; and things in motion tend to remain in motion and to resist change. Importantly, different parts of the same object can have different inertias. The larger the part and the more it weighs, the larger the inertia, or the greater its tendency to not want to change its state of rest or its state of motion.
The object in question in a whiplash injury is a human body. The human body has two large parts that have their own separate inertia, the trunk and the head. These two large pieces of inertial mass (the head and the trunk) are connected by the cervical spine. It is aspects of the cervical spine that are vulnerable to inertial injuries during motor vehicle collisions.
During a rear-end motor vehicle collision, the vehicle that is struck from behind will quickly move forward. As the vehicle moves forward, so do the passenger seats in the vehicle. As the passenger seat moves forward, so does the trunk of the passenger sitting in the seat. However, the head of the passenger in the seat does not move forward because the head has a separate inertia from the trunk. As the vehicle, the seat, and the trunk move forward from the collision, the head remains at rest, forcing the neck backwards. The result is an inertial injury to the soft tissues of the joints of vertebrae the cervical spine. Importantly, the neck does not hit anything; it sustains an inertial injury, similar to that seen in shaken baby syndrome. This injury involves no physical contact; rather, the injury is inertial.
Much of the rear-end collision inertial injury can be avoided or minimized if the vehicle has an adequate head restraint (head rest). With an adequate head restraint, the vehicle, seat, passenger trunk, passenger neck, and passenger head, will move forward together, eliminating or reducing inertial stress and inertial injury to the cervical spine. It is established that the best head restraint to prevent these inertial injuries to the cervical spine is one that is both high (above the center of mass of the skull), and close to the back of the skull. In fact, the very best head restraint is when the head is actually resting on the head restraint at the time of vehicle impact. Importantly, head restraints that are more than one inch behind the skull at the time of vehicle impact have been shown to be inadequate for the purposes of preventing cervical spine inertial injuries from rear-end collisions. Studies have shown that as much as 90% of head restraints in vehicles are inadequate to effectively prevent hyperextension inertial injuries produced by rear-end motor vehicle collisions. I recently saw an early model Ford Mustang, and I am reminded that there are still millions of vehicles on the road that have no head restraint at all.
During a head-on motor vehicle collision, the principle of inertia and inertial injury still apply. As an example, if a vehicle is traveling at 25 mph, the occupant’s trunk, head, and neck are also traveling at 25 mph. If that vehicle runs into a solid wall or tree, the vehicle abruptly stops. However, in accordance with Newton’s Law of Inertia, the trunk, head, and neck of the occupant continue to move forward at 25 mph. If such occupant is not wearing a seat belt and the occupant position is not equipped with an air bag, the occupant’s entire body (trunk, head, and neck) will be thrown forward at 25 mph, crashing into the dash or windshield of the vehicle, including possible ejection through the front windshield. The contact injuries sustained are usually serious to fatal.
During this head-on motor vehicle collision, if the occupant is wearing a seat belt, the primary injuries sustained change from inertial contact injuries to inertial non-contact injuries, as follows:
Initially, after vehicle contact with the wall or tree, the occupant’s entire body (trunk, head, and neck) will be thrown forward as a single inertial unit at 25 mph. Within a fraction of a second, the shoulder harness and lap portion of the seat belt will engage, effectively stopping the forward motion of the trunk of the occupant’s body. This will usually prevent the trunk from hitting the dash or windshield, and ejection of the body from the vehicle. However, in accordance with the Law of Inertia, the head will continue to move forward at a rate of 25 mph. The result is a tremendous inertial load and injury to the structures of the cervical spine.
Head-on vehicle collisions that create a certain amount of mechanical deformation to the front of the vehicle will initiate a rapid cascade of events that initiates the deployment of the air bags. Airbag deployment is an important advancement in the technology designed to protect the neck from inertial stress and injury during a motor vehicle head-on collision. Airbags reduce the forward motion of the head with respect to the trunk, thus sparing inertial loading to the cervical spine. Sadly, usually only the vehicle driver and front seat passenger enjoy the added protection from air bag deployment. Other passengers are not so protected. In addition, air bags themselves have been found to injure vehicle passengers as a consequence of their rapid deployment. Studies have found that short stature persons, who must move their seats forward to effectively operate the vehicle, and children, are most vulnerable to airbag deployment injuries.
II
What is Injured in a Whiplash Injury?
The spinal vertebrae joint ligaments, muscles, and the disc joint are collectively known as soft tissues.
Although whiplash trauma inertial injury can fracture a bone(s) of the cervical spine, herniate an intervertebral disc, damage cervical spine nerve roots, and/or damage the cervical spine spinal cord, such injuries are relatively rare. Much more common is injury to the cervical spine soft tissues. These soft tissue injuries are primarily found in the muscles, the ligaments, and the facet joint capsule. Intervertebral disc injuries also occur, but it is not common for the disc injury to be classified as a herniation. Again, these injuries are classified as soft-tissue injuries.
III
What are the Stages for the Healing of Injured Soft Tissues?
There is a lot of misunderstanding regarding soft tissue injury and its repair. The most common misconception is that injured soft tissue will heal in a period of time between four and eight weeks. Frequently it is claimed that injured soft tissues will heal spontaneously, leaving no long-term residuals, and that treatment is not required. This type of information is very misleading and confusing.
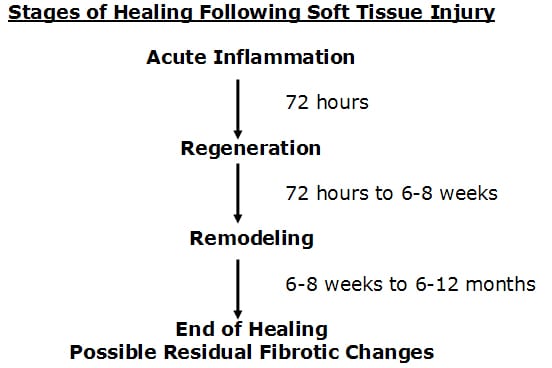
Published articles and books concerning the healing of injured soft tissues indicate that the academic time frame for such healing is approximately one year. Healing takes place in three specific phases:
1) The acute inflammatory phase:
This phase will last approximately 72 hours. During this phase, there is initial bleeding and continual associated inflammation of the injured tissues. Because of the increasing inflammatory cascade during this period of time, it is not uncommon for the patient to feel worse for each of the first three days following injury. Because the injury causes a disruption of local vascular supplies, there is insufficient availability of substrate (glucose, oxygen, etc.) to produce large enough quantities of ATP energy to initiate collagen protein synthesis to repair the wound.
2) The regeneration or proliferation phase:
After about 72 hours following injury, the damaged blood vessels have mended. The resulting increased availability of glucose and oxygen elevates local ATP levels and collagen repair begins by the fibroblasts that accumulated during the acute inflammatory phase. During this regeneration phase, the disruption in the injured muscles and ligaments is bridged. The fibroblasts manufacture and secrete collagen protein glues that bridge the gap in the torn tissues. This phase will continue for approximately 6-8 weeks. At the end of 6-8 weeks, the gap in the torn tissues is more than 90% bridged. Many will erroneously claim this to be the end of healing. However, it clearly is not. There is a third and final phase of healing.
3) The phase of remodeling:
The phase of remodeling begins near the end of the phase of regeneration. During the phase of remodeling the collagen protein glues that have been laid down for repair are remodeled in the direction of stress and strain. This means that the fibers in the tissue will become stronger, and will change their orientation from an irregular pattern to a more regular pattern, a pattern more like the original undamaged tissues. Proper treatment during this remodeling phase is very necessary if the tissues are to get the best end product of healing. It is during this remodeling phase that the tissues regain strength and alignment. Remodeling takes approximately one year after the date of injury. It is established that remodeling takes place as a direct byproduct of motion. Chiropractic healthcare puts controlled motion into the tissues in an effort at getting them to line up along the directions of stress and strain, thereby giving a stronger, more elastic end product of healing.
Published studies and experience shows that the most effective management of injured soft tissues involves early, persistent, controlled motion into the injured tissues. The proper application of this art requires both training and experience. The intuition of the provider in introducing this controlled motion is necessary. Classically the motion is carefully applied and remains within the limits of pain for the individual patient. Any exacerbation of symptoms is usually an indication that the prior motion efforts were excessive and the provider should “slow down.”
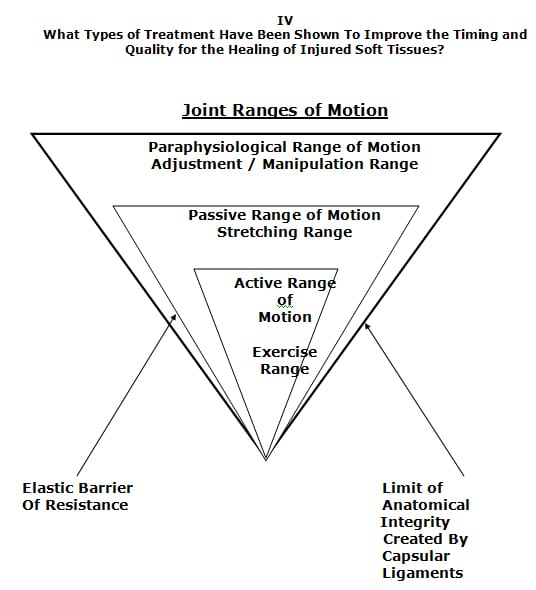
As noted in the drawing above, therapeutic motion for the management of injured soft tissues is divided into three categories:
1) Active Motion:
Active motion is the range that is actively influenced by the patient, by putting the involved tissues through a conscious range of motion and/or performing certain exercises. Although therapeutically beneficial, active motion only influences the narrowest range of the injured tissues.
2) Passive Motion:
Although the passive range of motion can be accessed by the patient through stretching-type exercises, this range is often more effectively accessed by the chiropractor or other provider who would gently, carefully and intuitively push the injured tissues further than the patient can do with active range of motion exercises. As noted, moving into the passive range of motion influences a larger range of injured tissues, enhancing the timing and degree of patient recovery. In addition, a skilled provider has the training and skills to isolate the joints and tissues that are injured and hypomobile, concentrating therapeutic efforts to those tissues, and thus improving outcomes.
3) Periarticular Paraphysiological Space Motion:
The final range of motion has been termed the Periarticular Paraphysiological Space Motion. Traditional chiropractic joint manipulation healthcare is directed towards putting motion into the periarticular paraphysiological space. The concept of paraphysiological joint motion was first described in the 1970s, and this concept has endured for decades. Today, the concept of chiropractic joint manipulation healthcare putting motion into the periarticular paraphysiological space is found in both chiropractic and medical reference books and journal articles. These discussions clearly show that there is a component of motion that cannot be properly addressed by exercise, stretching, massage, etc, but that this component of motion can be properly addressed by osseous joint manipulation. Therefore, traditional chiropractic osseous joint manipulation adds a unique aspect to the treatment and the remodeling of periarticular soft tissues that have sustained an injury.
The traditional approach to introducing motion into the periarticular paraphysiological space involves the chiropractor moving the appropriate joint through the active range and into the passive range of motion. At the end of the passive range of motion there is a specific feel that indicates the need and safety for the introduction of additional movement. This specific feel is referred to as The Elastic Barrier of Resistance. When the additional movement is so indicated, the chiropractor skillfully pushes the involved joint through the elastic barrier of resistance and in so doing enters the final range of motion, the Periarticular Paraphysiological Space Motion. The crossing of the elastic barrier of resistance into the periarticular paraphysiological space motion is usually associated with an audible and palpable cracking noise. This constitutes a chiropractic spinal adjustment. It is important to note that this spinal adjustment does not cross the limit of anatomical integrity, which is created by the capsular ligaments. This means that the adjustment does not cause any additional soft tissue stress.
Over the decades, a number of studies have compared the management of injured soft tissues by early mobilization vs. immobilization. These studies have revealed a clear advantage to early mobilization. Early mobilization has been shown to benefit the healing of injured soft tissues, as follows:
- Early mobilization promotes a more rapid return to full activity.
- Early mobilization promotes a more rapid return to full functional recovery.
- With early mobilization, the stress of movement on the repairing collagen improves the orientation and tensile strength of the tendons, ligaments, and muscles.
- Early mobilization improves the strength of bone and ligament, which reduces recurrence of injury.
- The strength of repaired ligaments is proportional to the mobility of the ligament, and early mobilization results in larger diameter collagen fiber bundles and more total collagen.
- Collagen fiber growth and realignment is stimulated by early tensile loading of muscle, tendon, and ligament as a consequence of early mobilization.
- With early mobilization, fewer adverse adhesions develop between repairing tissues and adjacent structures.
- With early motion, joint proprioception is maintained or develops earlier after injury, and this reduces recurrences of injuries and hastens full recovery.
- The nutrition to the cartilage is better maintained with early mobilization.
What Types of Treatment Have Been Shown to be Detrimental to the Timing and Quality in the Healing of Injured Soft Tissues?
In contrast, immobilization has been shown to be deleterious to the healing process, as follows:
1) Immobilization causes muscle wasting, atrophy, and loss of strength.
2) Immobilization increases the development of adverse granulation, fibrotic, or scar tissue. This causes the joint stiffness that is often responsible for prolonged disability and pain.
What Problems Are Associated With the Healing of Injured Soft Tissues?
There are some problems associated with the healing of injured soft tissues. Despite the best of management, microscopic histological studies show that the repaired tissue is different than the original, adjacent, undamaged tissues. Specifically, the repaired tissue is often plagued with residual granulation, scar, or fibrotic residuals. This fibrotic residual that develops subsequent to soft tissue trauma may create problems that adversely affect the tissues and the patient for years, decades, or even forever. This is because the fibrosed tissues are functionally different from the adjacent normal tissues. The differences fall into three main categories:
1) The fibrotic repaired tissue is weaker and less strong than the undamaged tissues. This is because the diameter of the healing collagen fibers is smaller, and the end product of healing is deficient in the number of crossed linkages within the collagen repair.
2) The fibrotic repaired tissue is stiffer or less elastic than the original, undamaged tissues. This is because the healing fibers are not aligned identically to that of the original tissue. Examination range of motion studies show there are areas of decrease of the normal joint ranges of motion.
3) Fibrous repair tissue is capable of maintaining an inflammatory response long after the initial cause has ceased to operate. Since inflammation alters the thresholds of the nociceptive afferent system, physical examinations in these cases will show these fibrotic areas display increased sensitivity, and digital pressure may show hypertonicity and spasm.
Because the fibrotic residuals have rendered the tissues weaker, less elastic, and more sensitive, the patient will have a history of flare-ups of pain and/or spasm at times of increased use or stress. These episodes of pain and/or spasm at times of increased use or stress of the once damaged soft tissues are often a problem that the patient will have to learn to live with. These exacerbations of pain and/or spasm may continue for an indefinite period of time in the future, and the patient may have a need for additional treatment for these episodes of pain and/or spasm.
How Often Should the Whiplash Injured Patient be Treated?
Although the frequency of treatment for the injured whiplash patient should probably be determined on an individual case basis, some general recommendations have appeared in the whiplash trauma literature. For nearly six decades, the whiplash literature has shown remarkable consistency in suggesting the initial frequency for early mobilization management. The basic suggestion is that the acutely injured whiplash patient should be treated with early persistent controlled mobilization of the injured soft tissues. Initially the treatment frequency should be daily for a period of about two weeks. Starting in the third week following injury, the treatment frequency can be reduced to about three times per week, and this should continue for a period of about four weeks. Following this, treatment frequency can be reduced to twice per week for about an additional 10 weeks, depending on the needs of the individual patient.
Published studies indicate that range of duration in time for the whiplash-injured patient to reach maximum improvement of clinical status is from about two months to about two years. It is very clear that some whiplash-injured patients require two years of treatment to achieve maximum improvement.
Do All Whiplash-Injured Patients Fully Recovery
There are many long-term studies looking at the improvement outcome of whiplash-injured patients. Each of the studies report different statistics for recovery rates, but essentially they average that around 25% will suffer from long-term subjective and objective residuals that interfere with their work and leisure activities. These long-term residuals appear to be permanent injuries that the patient will have to learn to live with. Importantly, these residuals persist even after the patient has obtained all possible financial compensation, implying that these residuals are not secondary to compensation status or desire.
Summary
It appears that early persistent mobilization of the injured soft tissues is the superior management for the management of whiplash injuries. The modern chiropractor is extensively trained in the application of the early mobilization, exercise, and manipulation techniques to properly manage both the acute and chronic whiplash-injured patient. The application of these management techniques physiologically induce the following:
1) Dispersion of the accumulation of inflammatory exudates that increase pain. This accelerates the timing of the healing process and improves the quality of the end product of healing.
2) The application of controlled motion into the developing granulation tissue. This helps in the alignment of the tissues in the directions of stress and strain. This improves the quality of the end product of healing, reducing the chances that future increased stress will result in an exacerbation of signs and symptoms.
3) Reduces the formation of adhesions that often cause prolonged disability after soft tissue injury and healing.
4) Reduces the quantity of fibrotic tissue. This improves function, reducing the incidence of exacerbations of pain and/or spasm at times of increased use or stress.
5) A uniqueness to the chiropractic approach to the management of these soft tissue injuries is the utilization of specific line-of-drive joint manipulation (chiropractic adjustment). The chiropractic adjustment has the advantage of non-traumatically moving the injured tissues into the periarticular paraphysiological space range of motion. The additional range of motion achieved with spinal adjusting improves injured tissue healing and remodeling, resulting in improved clinical outcomes.
Several studies have shown the benefits of chiropractic spinal adjusting in the management of whiplash injury soft tissue trauma. These studies are important because the patients involved had already failed to improve with other more traditional approaches that did not include joint manipulation.