Our government (United States of America) collects and owns what experts consider to be reputable biomedical healthcare literature. This literature is catalogued in a library that is physically located in Bethesda, Maryland. The name of the library is The National Library of Medicine. The biomedical journals of the entire world can be found in our National Library of Medicine.
Our National Library of Medicine has collected and catalogued more than 20 million citations, and thousands more are added every day. One can access this database of citations by using a search engine that is commonly referred to as PubMed (www.pubmed.gov). Anyone with Internet access can use PubMed to search the biomedical contents of our National Library of Medicine by simply typing in any health topic into the search bar such as “whiplash” or “vitamin D” or “fibromyalgia” or thousands of other topics. The literature that is pulled up from searching the National Library of Medicine is always the most technical in the world, meaning that it is geared for health care professional and researchers, not for introductory knowledge that may appeal to lay people (even though anyone can access this information).
••••
Electrons are negatively charged particles that spin around the nucleus of atoms. The different orbits of these spinning electrons are called shells. The biochemistry and physiology of life is often linked to events occurring with the electrons in the outer shells of atoms. The donation or sharing of these outer shell electrons expedites the efficiency of most human physiological processes.
The spinning electrons like to exist in pairs. Atoms and/or molecules are stable when the outer shell electrons are in even numbers. If something happens to the outer shell electrons (like adding or subtracting an electron) so that an odd number of electrons exist, the atom/molecule becomes unstable, and in general, this is not good. This unstable atom/molecule is called a Free Radical. Free Radicals can damage adjacent atoms/molecules by disrupting their compliment of outer shell electrons, creating deleterious things such as mutations and toxic substances.
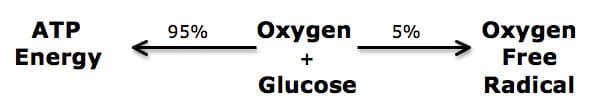
The most notorious of the Free Radicals are Oxygen Free Radicals. This is because Oxygen Free Radicals are produced as a normal byproduct of respiration, the creation of ATP energy molecules from glucose and oxygen in the inner membrane of the mitochondria. All of us make these Oxygen Free Radicals continually throughout our life, from birth until death. The only way to stop the production of these Oxygen Free Radicals is to stop breathing.
Healthy people make more ATP Energy than Oxygen Free Radicals. However, the damage caused by Oxygen Free Radicals accumulates throughout our lives. This accumulated damage includes damage to the mitochondrial machinery. As the mitochondria are progressively damaged by Oxygen Free Radicals, they produce less and less ATP Energy and more and more Oxygen Free Radicals, thus a vicious cycle of damage ensues.
This example is that of a relatively healthy person; 95% of the oxygen and glucose is converted into ATP Energy, while 5% is converted into Oxygen Free Radicals:
Oxygen Free Radicals are technically called Reactive Oxygen Species and are commonly abbreviated ROS. When a tissue is damaged by a Free Radical, that tissue is declared to be Oxidized or to have sustained Oxidative Injury or Oxidative Stress.
••••
One of the best-documented concepts in health care is the Free Radical Theory of Aging. The vicious cycle of,
Mitochondria produce Oxygen Free Radicals
Oxygen Free Radicals damage the mitochondria (Oxidized mitochondria)
Oxidized mitochondria produce more Oxygen Free Radicals and simultaneously produce less ATP energy, accelerating the aging process
accounts for the deleterious nature of Free Radicals and ageing.
When researching the Free Radical Theory of Aging, using the technical words “Reactive Oxygen Species” is a good way to start. Typing the words “reactive oxygen species” into the PubMed search bar (12/07/11) called up 116,200 articles from the National Library of Medicine. The words “reactive oxygen species AND ageing” in the PubMed search bar produced 7,662 articles. The words “reactive oxygen species AND osteoarthritis” in the PubMed search bar produced 175 articles.
The consensus among these articles is that Free Radical damage is an important contributor to osteoarthritis. A few examples of this include:
- In December 2009, the Journal of the Medical Association of Thailand published an article titled (Sutipornpalangkul):
Free Radicals in Primary Knee Osteoarthritis
The abstract of this article includes:
“Free radicals have an important role in the pathogenesis of knee osteoarthritis. Reactive oxygen species (ROS) produced by abnormal chondrocyte metabolism exceeds the physiological buffering capacity and results in oxidative stress. The excessive production of ROS can damage proteins, lipids, nucleic acids, and matrix components. They also serve as important intracellular signaling molecules that amplify the inflammatory response. An understanding of oxidative stress involved in this disease might allow the use of antioxidant therapies in the prevention and/or treatment of knee osteoarthritis.”
- In September 2010, the journal Orthopedic Reviews published an article titled (Ziskoven):
Oxidative stress in secondary osteoarthritis: from cartilage destruction to clinical presentation?
The abstract of this article includes:
“Due to an increasing life expectance, osteoarthritis (OA) is one of the most common chronic diseases.”
“The dysbalance between free radical burden and cellular scavenging mechanisms defined as oxidative stress is a relevant part of OA pathogenesis.”
“Free radical exposure is known to promote cellular senescence and apoptosis. Radical oxygen species (ROS) involvement in inflammation, fibrosis control and pain nociception has been proven. The data from literature indicates a link between free radical burden and OA pathogenesis mediating local tissue reactions between the joint compartments. Hence, oxidative stress is likely not only to promote cartilage destruction but also to be involved in inflammative transformation, promoting the transition from clinically silent cartilage destruction to apparent OA.”
“ROS induced by exogenous factors such as overload, trauma, local intra-articular lesion and consecutive synovial inflammation cause cartilage degradation. In the affected joint, free radicals mediate disease progression. The interrelationship between oxidative stress and OA etiology might provide a novel approach to the comprehension and therefore modification of disease progression and symptom control.”
- In September 2011, the journal Current Opinion in Rheumatology published an article titled (Loeser):
Aging and Osteoarthritis
The abstract of this article includes:
“Osteoarthritis is strongly linked to aging but the mechanisms for this link are incompletely understood.”
“Cell stress or cell damage response contributes to chronic inflammation that promotes age-related diseases. This cellular response results in the senescence-associated secretory phenotype which has many of the characteristics of an osteoarthritic chondrocyte in terms of the cytokines, chemokines, and proteases produced. Oxidative stress can promote cell senescence and studies have shown a role for oxidative stress in altering cell signaling pathways in chondrocytes that can disrupt the response to growth factors. Mitochondria are an important source of reactive oxygen species and studies continue to support a role for the mitochondria in osteoarthritis, including work suggesting changes in energy production.”
My favorite article pertaining to osteoarthritis and free radical damage was published in the American Journal of Physical Medicine and Rehabilitation in 2006, titled (Garstang):
Osteoarthritis
Epidemiology, Risk Factors, and Pathophysiology
The authors, Susan V Garstang, MD and Todd P Stitik, MD, are from the University of Medicine and Dentistry of New Jersey. In this article, Drs. Garstang and Stitik note that osteoarthritis is:
“the clinical and pathologic outcome of a range of disorders that results in structural and functional failure of synovial joints. Osteoarthritis occurs when the dynamic equilibrium between the breakdown and repair of joint tissues is overwhelmed.”
Drs. Garstang and Stitik note that osteoarthritis is the most prevalent form of arthritis and a major cause of disability in people aged 65 and older. Osteoarthritis affects the majority of adults over age 55.
Garstang and Stitik note that the incidence of osteoarthritis is influenced by both systemic and local factors. Important to this discussion, Drs. Garstang and Stitik note that pertaining to systemic factors, that there is evidence that osteoarthritis is linked to free radicals, and that high dietary antioxidants (especially vitamins C and D) are protective against the development of osteoarthritis. They state: “Chondrocyte senescence is thought to be the result of chronic oxidative stress.”
Garstang and Stitik note that if elevated oxidative stress systemic factors are present, the joints are vulnerable, and thus local biomechanical factors will have more of an impact on joint degeneration and osteoarthritis. Historically, traditional chiropractic patient management emphasizes the treatment and resolution of the local biomechanical factors which are undoubtedly factors in the genesis and progression of joint osteoarthritis. Considering the impact of Free Radicals and Oxidative Stress as systemic influences on joint degeneration and osteoarthritis is an important addition to the management of these patients.
••••
Turning our discussion to Free Radicals and Oxidative Stress, an authoritative text on the subject is the book:
Oxidative Stress, Disease and Cancer
This book is edited by Keshav K. Singh of the Roswell Park Cancer Institute in New York. This 2006 reference book has more than 1,000 pages of information.
A central theme of this book is that free radicals and inflammation are intimately linked: free radicals drive inflammation and inflammation drives free radicals. This book lists six (6) primary drivers of the production of Reactive Oxygen Species (ROS). They are:
1) The arachidonic acid cascade to inflammatory prostaglandins and leukotrienes.
2) The glutamate cascade.
3) Low antioxidant defenses.
4) Excessively high metabolic activities.
5) High levels of metal toxins, such as iron and copper.
6) Increased production and release of catecholamines.
Discussing aspects of each of these six drivers of Reactive Oxygen Species is relevant to his discussion:
1) The arachidonic acid cascade to inflammatory prostaglandins and leukotrienes.
Arachidonic acid is a 20-carbon long omega-6 fatty acid. It is a metabolic
precursor to the powerfully pro-inflammatory eicosanoid prostaglandin
(PGE2) and leukotriene (LTB4) hormones. Dr. Singh describes how these pro-inflammatory eicosanoid arachidonic acid derivatives increase the production Oxygen Free Radicals which would systemically contribute to joint osteoarthritis.
The biochemical anti-inflammatory nemesis of arachidonic acid is the omega-3 fatty acid eicosapentaenoic acid. Eicosapentaenoic acid produces anti-inflammatory eicosanoid hormones, stopping cartilage degradation and osteoarthritis (Curtis).
Cyclo-oxygenase (COX)/Lipo-oxygenase (LOX) Pathways
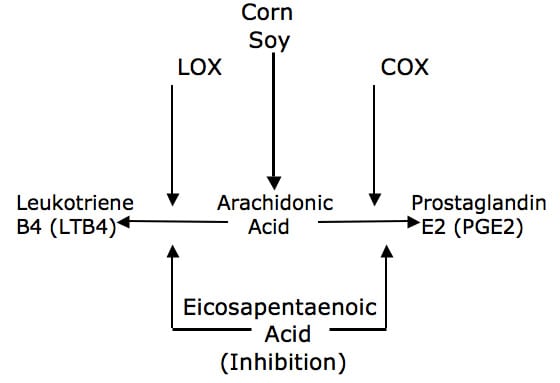
The 2006 book Weiner’s Pain Management, A Practical Guide for Clinicians (Boswell) notes that Paleolithic humans evolved with a ratio of
omega-6/omega-3 of about 1/1, but that contemporary ratios are often as high as 25/1. This ratio is pro-inflammatory and drives the production of Free Radicals, leading to osteoarthritis.
2) The glutamate cascade.
Glutamic acid (glutamate) is an amino acid. It is also the primary excitatory neurotransmitter for the nervous system. Recently retired neurosurgeon Russell Blaylock, MD, describes in his 1997 book Excitotoxins, The Taste That Kills, how glutamate excites pain, excites the production of Free Radicals, and also excites taste. As a consequence of its taste enhancing qualities, glutamate is added to nearly all processed and packaged foods. It is classically labeled as monosodium glutamate or MSG, but Dr. Blaylock notes that manufacturers usually change the name to literally a few dozen different words, such as hydrolyzed vegetable protein. A more complete list of these other names appears in the back of Dr. Blaylock’s book, and I have included a list from the webpage www.truthinlabeling.org at the end of this article.
There are studies on chronic pain patients who abstain from all sources of free glutamic acid for four months becoming completely cured of their pain complaints (Smith).
Once again, Dr. Singh describes how the glutamate cascade increases the production of Oxygen Free Radicals which would systemically contribute to joint osteoarthritis.
3) Low antioxidant defenses.
Free Radicals damage many tissues, including joint cartilage, leading to and accelerating osteoarthritis. Yet, these Free Radicals can be neutralized prior to causing tissue damage. Molecules termed Antioxidants do this neutralization. Our exogenous antioxidant defenses are dependent upon the quality of our habitual eating habits. Fruits and vegetables are particularly rich in antioxidants. Their ability to neutralize Free Radicals could reduce the oxidative damage to the joint, preventing or minimizing osteoarthritis.
Sadly, a 2009 study by the United States Centers for Disease Control (Anderson) found that only 14% of US adults and 9.5% of high school students consumed the daily-recommended portion of fruits and vegetables. This suggests that anti-oxidant supplementation may be necessary for a large portion of the US population.
4) Excessively high metabolic activities.
Although most Americans do not exercise regularly, most Americans do believe that exercise is good for health. However, exercise is a paradox.
Aerobics began in 1968 by cardiologist Kenneth Cooper, MD. Yet, in 1994, Dr. Cooper wrote the book Dr. Kenneth Cooper’s Antioxidant Revolution. In this book, Dr. Cooper notes that excessive exercise produces excessive Free Radicals, damaging tissues, and the greater the exercise level the greater the need for supplemental anti-oxidants. His book notes:
Free radicals—or unstable oxygen molecules, also known as reactive oxygen species—are implicated in more than 50 diseases including cancer, heart disease, premature aging, cataracts and AIDS.
Free radicals are central actors in most human disease.
Too much exercise may actually increase the risk of developing medical problems.
I strongly recommend the use of antioxidants on a regular basis, regardless of the level of physical activity.
“The more the body is exposed to free radicals, the shorter the life span will be.”
The body’s increased need for oxygen during exercise increases the production of free radicals which oxidize the fats in muscle cell membranes, making muscle cells susceptible to aging and other damage.
“To build strong protection against free radicals, you need to take far larger amounts of antioxidants than the official RDA provides.”
The degenerative changes associated with aging are caused by an accumulation of free radical damage.
An antioxidant is any substance that protects tissues from oxidative damage.
“It is absolutely necessary that you fortify your body’s natural defenses with exogenous antioxidants.”
The bottom line is that excessive exercise increases the genesis of destructive Oxygen Free Radicals, and this problem is magnified if one has poor anti-oxidant defenses.
5) High levels of metal toxins, such as iron and copper.
Excessive metal ions are toxic to our bodies because they increase the production of Free Radicals. The sources of these toxic metals are too many to list (Cranor). Although complete avoidance is impossible, common sense and knowledge can reduce our exposures to metal toxins, reduce the genesis of Oxygen Free Radicals, and reduce their impact on our bodies, including osteoarthritis.
Some of these common sense and knowledge strategies include:
- Arsenic in chicken (The Meat You Eat, Midkiff, 2004)
- Mercury in fish (Diagnosis Mercury, Jane Hightower, 2009)
- Copper in municipal water and in supplements (Brewer, Journal of the American College of Nutrition, 2009)
Strategies to reduce adverse toxic metal ions include avoidance and detoxification (briefly described below).
6) Increased production and release of catecholamines.
Catecholamines are our stress hormones such as epinephrine and norepinephrine. Dr. Singh describes how the chronic increase production and release of catecholamines drives the production of Oxygen Free Radicals.
In 1953, Leonard Hayflick, PhD, anatomy professor at the University of California, San Francisco, discovered that human cells divided about 50 times, and then die. This is known as the Hayflick limit. Dr. Hayflick continues to research and publish on human aging and longevity.
About 30 years ago, scientists discovered the reason for the Hayflick limit was telomeres. Telomeres are short caps of DNA on the ends of chromosomes. Each time the cell divides, the telomere shortens a little. When most of the telomere disappears, the cell dies. Consequently, telomere length has been proposed as a marker of biological aging.
In 2004, the Proceedings of the National Academy of Sciences of the United States of America (Epel) published a study indication that chronic stress significantly shortens the telomeres. Elizabeth Blackburn, the second author of the study, was awarded the 2009 Nobel Prize in medicine/physiology for her work on telomeres.
In 2009, a study published in the American Journal of Clinical Nutrition noted that daily supplementation with a quality antioxidant multi-vitamin/mineral resulted in significantly longer telomeres (Xu). This suggests that quality antioxidant multi-vitamin/mineral supplementation counteracts the effects of chronic stress and catecholamines.
In 2010, a study published in the Journal of the American Medical Association noted that omega-3 fatty acid consumption also resulted in significantly longer telomeres (Farzaneh-Far). This is consistent with the arachidonic acid cascade from #1 above, suggesting that the anti-inflammatory benefit of omega-3 fatty acids also counteracts the effects of chronic stress and catecholamines.
••••
Summary and Conclusions
The core of chiropractic management of patients suffering from osteoarthritis will continue to emphasize mechanical aspects of the condition. This includes addressing problems with articular alignment, problems with motion/movement patterns, and problems with joint mechanoreception/proprioception.
However, the information presented here indicates that patients with these joint mechanical problems have greater vulnerability to develop osteoarthritis in the presence of increased Oxidative Stress. Following the lead of Singh, our total management of these patients should include approaches to minimize the generation of Reactive Oxygen Species and its consequent Oxidative Stress. These strategies would include:
- Balancing the omega-6/omega-3 fatty acid ratio through diet or supplementation.
- Minimizing dietary consumption of glutamate (MSG) from processed and packaged foods. This would include becoming familiar with the many hidden names for free glutamic acid on food labeling (see the list at the end of this article from www.truthinlabeling.org).
- Eat a minimum of 5 servings of fruits and vegetables daily (2 fruits, 3 vegetables. Use a quality anti-oxidant multi-vitamin/mineral supplement daily (just be sure that it has no more than 100 micrograms of copper).
- Do not over exercise. Regular moderate exercise is good and acceptable. The more one exercises, the more one needs to rely on anti-oxidant supplements.
- Avoid well-published sources of metal ion toxins, such as some fish (mercury), chicken (arsenic), municipal water (copper), and many multi-vitamin/mineral supplements (copper). Read the book Legally Poisoned, How the Law Puts Us at Risk of Toxicants by Carl Cranor, 2011.
- Detoxify by elevating levels of glutathione and using infra-red saunas. Read Glutathione, Your Body’s Most Powerful Healing Agent by Jimmy Gutman, MD, 2008. Read Detoxify or Die by Sherry Rodgers, MD, 2002.
- Minimize both physical and emotional stress.
REFERENCES:
Sutipornpalangkul W, Morales NP, Harnroongroj T; Free radicals in primary knee osteoarthritis; Journal of the Medical Association of Thailand; December 2009 Dec; Vol. 92; Supplemental 6:S268-74.
Ziskoven C, Jager N, Zilkens C, Bloch W, Brixius K, Krauspe R; Oxidative stress in secondary osteoarthritis: from cartilage destruction to clinical presentation? Orthopedic Reviews; September 23, 2010;Vol. 2; No. 2; pp. e23.
Loeser RF; Aging and osteoarthritis; Current Opinion in Rheumatology; September 2011; Vol. 32; No. 5; PP. 492-496.
Garstang SV, Stitik, TP; Osteoarthritis: Epidemiology, Risk Factors, and Pathophysiology; American Journal of Physical Medicine and Rehabilitation; November 2006, Vol. 85, No. 11, pp. S2-S11.
Singh KK; Oxidative Stress, Disease and Cancer; Imperial College Press; 2006.
Curtis CL, Rees SG, Little CB, Flannery CR, CHughes CE, Wilson C, Dent CM, Otterness IG, Harwood JL, Caterson B; Pathologic indicators of degradation and inflammation in human osteoarthritic cartilage are abrogated by exposure to n-3 fatty acids; Arthritis & Rheumatism; Volume 46, Issue 6, 2002, pp 1544-1553.
Boswell M and Cole BE; Weiner’s Pain Management; A Practical Guide for Clinicians; American Academy of Pain Management; Seventh Edition, 2006, pp.584-585.
Blaylock R; Excitotoxins, The Taste That Kills, Health Press, 1997.
Smith JD, Terpening CM, Schmidt SOF, Gums JG; Relief of Fibromyalgia Symptoms Following Discontinuation of Dietary Excitotoxins; The Annals of Pharmacotherapy: Vol. 35, No. 6, pp. 702–706; June 2001.
Anderson L; US Diets Fall Short on Fruit, Vegetables; USA Today; September 30, 2009.
Cooper K; Dr. Kenneth Cooper’s Antioxidant Revolution; Thomas Nelson Publishers; 1994.
Midkiff K; The Meat You Eat: How Corporate Farming Has Endangered America’s Food Supply; St. Martin’s Press, 2004
Hightower J; Diagnosis Mercury: Money, Politics, and Poison; Island Press, 2009.
Cranor C; Legally Poisoned, How the law Puts Us at Risk of Toxicants; Harvard University Press; 2011.
Brewer GJ; The Risks of Copper Toxicity Contributing to Cognitive Decline in the Aging Population and to Alzheimer’s Disease; Journal of the American College of Nutrition; June 2009, Vol. 28. No. 3, pp. 238-242.
Epel ES, Blackburn EH, Lin J, Dhabhar FS, Alder NE, Morrow JD, Cawthon RM; Accelerated telomere shortening in response to life stress; Proceedings of the National Academy of Sciences of the United States of America (PNAS); December 7, 2004, Vol. 101, No. 49 17312-17315.
Qun Xu, Christine G Parks, Lisa A DeRoo, Richard M Cawthon, Dale P Sandler and Honglei Chen; Multivitamin use and telomere length in women; American Journal of Clinical Nutrition; Vol. 89, No. 6, 1857-1863, June 2009, pp. 1857-1863.
Ramin Farzaneh-Far, MD, Jue Lin, PhD, Elissa S. Epel, PhD, William S. Harris, PhD, Elizabeth H. Blackburn, PhD, and Mary A. Whooley, MD; Association of Marine Omega-3 Fatty Acid Levels With Telomeric Aging in Patients With Coronary Heart Disease; Journal of the American Medical Association; January 20, 2010; Vol. 303 No. 3.
www.truthinlabeling.org
HIDDEN SOURCESOF PROCESSED FREE GLUTAMIC ACID (MSG)
Autolyzed, hydrolyzed, glutamate, glutamic acid, hydrolyzed, autolyzed
NAMES OF INGREDIENTS THAT CONTAIN ENOUGH MSG TO SERVE AS COMMON MSG-REACTION TRIGGERS
These ALWAYS contain MSG
Glutamate
Glutamic acid
Gelatin
Monosodium glutamate
Calcium caseinate
Textured protein
Monopotassium glutamate
Sodium caseinate
Yeast nutrient
Yeast extract
Yeast food
Autolyzed yeast
Hydrolyzed protein (any protein that is hydrolyzed)
Hydrolyzed corn gluten
These OFTEN contain MSG or create MSG during processing
Carrageenan
Maltodextrin
Malt extract
Natural pork flavoring
Citric acid
Malt flavoring
Bouillon and Broth
Natural chicken flavoring
Soy protein
Soy protein isolate
Anything fermented
Whey protein
Natural beef flavoring
Ultra-pasteurized
Soy sauce
Stock Barley malt
Soy sauce extract
Whey protein concentrate
Pectin
Protease
Natural flavor & flavoring
Soy protein concentrate
Whey protein isolate
Enzymes
Anything protein fortified
Flavors(s) & Flavoring(s)
Anything enzyme modified
Enzymes anything
Seasonings (the word “seasonings”)
The new game is to label hydrolyzed proteins as pea protein, whey protein, corn protein, etc.
If a pea, for example, were whole, it would be identified as a pea.
Calling an ingredient pea protein indicates that the pea has been hydrolyzed, at least in part, and that processed free glutamic acid (MSG) is present.
Relatively new to the list are wheat protein and soy protein.
